Abstract
Background
Sanitary sewage overflows (SSOs) release raw sewage, which may contaminate the drinking water supply. Boil water advisories (BWAs) are issued during low or negative pressure events, alerting customers to potential contamination in the drinking water distribution system.
Objective
We evaluated the associations between SSOs and BWAs and diagnoses of gastrointestinal (GI) illness in Columbia, South Carolina, and neighboring communities, 2013–2017.
Methods
A symmetric bi-directional case-crossover study design was used to assess the role of SSOs and BWAs on Emergency Room and Urgent Care visits with a primary diagnosis of GI illness. Cases were considered exposed if an SSO or BWA occurred 0–4 days, 5–9 days, or 10–14 days prior to the diagnosis, within the same residential zip code. Effect modification was explored via stratification on participant-level factors (e.g., sex, race, age) and season (January-March versus April-December).
Results
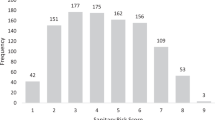
There were 830 SSOs, 423 BWAs, and 25,969 cases of GI illness. Highest numbers of SSOs, BWAs and GI cases were observed in a zip code where >80% of residents identified as Black or African-American. SSOs were associated with a 13% increase in the odds of a diagnosis for GI illness during the 0–4 day hazard period, compared to control periods (Odds Ratio: 1.13, 95% Confidence Interval: 1.09, 1.18), while no associations were observed during the other hazard periods. BWAs were not associated with increased or decreased odds of GI illness during all three hazard periods. However, in stratified analyses BWAs issued between January-March were associated with higher odds of GI illness, compared to advisories issued between April-December, in all three hazard periods.
Significance
SSOs (all months) and BWAs (January-March) were associated with increased odds of a diagnosis of GI illness. Future research should examine sewage contamination of the drinking water distribution system, and mechanisms of sewage intrusion from SSOs.
Impact
Sewage contains pathogens, which cause gastrointestinal (GI) illness. In Columbia, South Carolina, USA, between 2013–2017, there were 830 sanitary sewage overflows (SSOs). There were also 423 boil water advisories, which were issued during negative pressure events. Using case-crossover design, SSOs (all months) and boil water advisories (January-March) were associated with increased odds of Emergency Room and Urgent Care diagnoses of GI illness, potentially due to contamination of the drinking water distribution system. Lastly, we identified a community where >80% of residents identified as Black or African-American, which experienced a disproportionate burden of sewage exposure, compared to the rest of Columbia.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
SSO and BWA datasets are available from the corresponding author on reasonable request.
References
U.S. Environmental Protection Agency (USEPA). Report to Congress on Impacts and Control of Combined Sewer Overflows and Sanitary Sewer Overflows, EPA 833-R-04-001. 2004. https://www.epa.gov/sites/default/files/2015-10/documents/csossortc2004_full.pdf (last accessed October 19, 2022)
Jagai JS, Li Q, Wang S, Messier KP, Wade TJ, Hilborn ED. Extreme precipitation and emergency room visits for gastrointestinal illness in areas with and without combined sewer systems: an analysis of Massachusetts data, 2003–2007. Environ Health Perspect. 2015;123:873–9.
Redman, RL, Nenn, CA, Eastwood, D, Gorelick, MH. Pediatric emergency department visits for diarrheal illness increased after release of undertreated sewage. Pediatrics. https://doi.org/10.1542/peds.2007-0283 2007.
Alabama Center for Rural Enterprise (ACRE), The Columbia Law School Human Rights Clinic, The Institute for the Study of Human Rights at Columbia University. Flushed and Forgotten: Sanitation and Wastewater in Rural Communities in the United States. https://www.humanrightscolumbia.org/sites/default/files/Flushed%20and%20Forgotten%20-%20FINAL%20%281%29.pdf (last accessed October 19, 2022) 2019.
Craig DL, Fallowfield HJ, Cromar NJ. Use of microcosms to determine persistence of Escherichia coli in recreational coastal water and sediment and validation with in situ measurements. J Appl Microbiol. 2004;96:922–30.
Garzio-Hadzik A, Shelton DR, Hill RL, Pachepsky YA, Guber AK, Rowland R. Survival of manure-borne E. coli in streambed sediment: effects of temperature and sediment properties. Water Res. 2010;44:2753–62.
Shelton DR, Pachepsky YA, Kiefer LA, Blaustein RA, McCarty GW, Dao TH. Response of coliform populations in streambed sediment and water column to changes in nutrient concentrations in water. Water Res. 2014;59:316–24.
Ercumen A, Gruber JS, Colford JM Jr. Water distribution system deficiencies and gastrointestinal illness: a systematic review and meta-analysis. Environ Health Perspect. 2014;122:651–60.
Karim MR, Abbaszadegan M, LeChevallier M. Potential for pathogen intrusion during pressure transients. J Am Water Work Assoc. 2003;95:124–46.
LeChevallier MW, Gullick RW, Karim MR, Friedman M, Funk JE. The potential for health risks from intrusion of contaminants into the distribution system from pressure transients. J Water Health. 2003;1:3–14.
National Research Council (NRC). Drinking Water Distribution Systems: Assessing and Reducing Risks. 2006. https://www.nap.edu/catalog/11728/drinking-water-distribution-systems-assessing-and-reducing-risks (last accessed October 19, 2022).
Reynolds KA, Mena KD, Gerba CP. Risk of waterborne illness via drinking water in the United States. Rev Environ Contam Toxicol. 2008;192:117–58.
Teunis PFM, Xu M, Fleming KK, Yang J, Moe CL, LeChevallier MW. Enteric virus infection risk from intrusion of sewage into a drinking water distribution network. Environ Sci Technol. 2010;44:8561–6.
Hunter, PR, Chalmers, RM, Hughes, S, Syed, Q Self-reported diarrhea in a control group: a strong association with reporting of low-pressure events in tap water. Clin Infect Dis. https://doi.org/10.1086/427750 2005.
Lin GJ, Richardson DB, Hilborn ED, Weinberg H, Engel LS, Wade TJ. Emergency department visits for acute gastrointestinal illness after a major water pipe break in 2010. Epidemiology. 2019;30:893–900.
Nygård K, Wahl E, Krogh T, Tveit OA, Bøhleng E, Tverdal A, et al. Breaks and maintenance work in the water distribution systems and gastrointestinal illness: a cohort study. Int J Epidemiol. 2007;36:873–80.
South Carolina Department of Health and Environmental Control (SCDHEC). Wastewater (Sewer) Overflows. https://scdhec.gov/wastewater-sewer-overflows (last accessed October 19, 2022)
U.S. Environmental Protection Agency (USEPA). The United States of America and State of South Carolina v. The City of Columbia, 2013. https://www.epa.gov/sites/default/files/2013-09/documents/columbia-cd.pdf (last accessed October 19, 2022)
U.S. Census Bureau. American Community Survey, 5-Year Estimates, 2015-2019. 2022. https://data.census.gov/cedsci/ (last accessed October 19, 2022).
Brokamp C, Beck AF, Muglia L, Ryan P. Combined sewer overflow events and childhood emergency department visits: a case-crossover study. Sci Total Environ. 2017;607-608:1180–7.
Jagai, JS, DeFlorio-Barker, S, Lin, CJ, Hilborn, ED, Wade, TJ. Sanitary sewer overflows and emergency room visits for gastrointestinal illness: analysis of Massachusetts data, 2006-2007. Environ Health Perspect. https://doi.org/10.1289/EHP2048 2017.
Wade, TJ, Lin, CJ, Jagai, JS, Hilborn, ED. Flooding and emergency room visits for gastrointestinal illness in Massachusetts: a case-crossover study. PLoS One. https://doi.org/10.1371/journal.pone.0110474 2014.
Lin CJ, Wade TJ, Hilborn ED. Flooding and Clostridium difficile infection: a case-crossover analysis. Int J Environ Res Public Health. 2015;12:6948–64.
Emmons AM, Bizimis M, Lang SQ, Stangler W, Geidel G, Baalousha M, et al. Enrichments of metals, including methylmercury, in sewage spills in South Carolina, USA. J Environ Qual. 2018;47:1258–66.
Maclure M. The case-crossover design: a method for studying transient effects on the risk of acute events. Am J Epidemiol. 1991;133:144–53.
Maclure M, Mittleman MA. Should we use a case-crossover design? Annu Rev Public Health. 2000;21:193–221.
Lee, RM, Lessler, J, Lee, RA, Rudolph, KE, Reich, NG, Perl, TM, et al. Incubation periods of viral gastroenteritis: a systematic review. BMC Infect Dis, https://doi.org/10.1186/1471-2334-13-446 2013.
Drayna P, McLellan SL, Simpson P, Li S-H, Gorelick MH. Association between rainfall and pediatric emergency department visits for acute gastrointestinal illness. Environ Health Perspect. 2010;118:1439–43.
Wilson SM, Heaney CD, Cooper J, Wilson O. Built environment issues in unserved and underserved African-American neighborhoods in North Carolina. Environ Justice. 2008;1:63–72.
Kaufman JS, MacLehose RF. Which of these things is not like the other? Cancer. 2013;119:4216–22.
Hanley JA. A heuristic approach to the formulas for population attributable fraction. J Epidemiol Community Health. 2001;55:508–14.
Heaney C, Wilson S, Wilson O, Cooper J, Bumpass N, Snipes M. Use of community-owned and -managed research to assess the vulnerability of water and sewer services in marginalized and underserved environmental justice communities. J Environ Health. 2011;74:8–17.
Wade TJ, Sandhu SK, Levy D, Lee S, LeChevallier MW, Katz L, et al. Did a severe flood in the Midwest cause an increase in the incidence of gastrointestinal symptoms? Am J Epidemiol. 2004;159:398–405.
Gullick RW, LeChevallier MW, Svindland RC, Friedman MJ. Occurrence of transient low and negative pressures in distribution systems. J Am Water Work Assoc. 2004;96:52–66.
Marsili V, Meniconi S, Alvisi S, Brunone B, Franchini M. Experimental analysis of the water consumption effect on the dynamic behavior of a real pipe network. J Hydraul Res. 2021;59:477–87.
Yang J, LeChevallier MW, Teunis PFM, Xu M. Managing risks from virus intrusion into water distribution systems due to pressure transients. J Water Health. 2011;9:291–305.
Gibson, J, Karney, B, Guo, Y. Predicting health risks from intrusion into drinking water pipes over time. J Water Resour Plann Manage; https://doi.org/10.1061/(ASCE)WR.1943-5452.0001039 2019.
Calderon, JS, Verbyla, ME, Gil, M, Pinongcos, F, Kinoshita, AM, Mladenov, N. Persistence of fecal indicators and microbial source tracking markers in water flushed from riverbank soils. Water Air Soil Pollut. https://doi.org/10.1007/s11270-022-05542-8 2022.
Byappanahalli MN, Fujioka RS. Evidence that tropical soil environment can support the growth of Escherichia coli. Water Sci Technol. 1998;38:171–4.
Mika KB, Imamura G, Chang C, Conway V, Fernandez G, Griffith JF, et al. Pilot- and bench-scale testing of faecal indicator bacteria survival in marine beach sand near point sources. J Appl Microbiol. 2009;107:72–84.
Zimmer-Faust AG, Thulsiraj V, Marambio-Jones C, Cao Y, Griffith JF, Holden PA, et al. Effect of freshwater sediment characteristics on the persistence of fecal indicator bacteria and genetic markers within a Southern California watershed. Water Res. 2017;119:1–11.
Centers for Disease Control and Prevention (CDC). How Norovirus Spreads. 2021. https://www.cdc.gov/norovirus/about/transmission.html (last accessed October 19, 2022).
Navarro G, Sala RM, Segura F, Arias C, Anton E, Varela P, et al. An outbreak of norovirus infection in a long-term-care unit in Spain. Infect Control Hosp Epidemiol. 2005;26:259–62.
Centers for Disease Control and Prevention (CDC). E. coli (Escherichia coli). 2014. https://www.cdc.gov/ecoli/general/index.html (last accessed October 19, 2022)
Awofisayo-Okuyelu A, Hall I, Arnold E, Byrne L, McCarthy N. Analysis of individual patient data to describe the incubation period distribution of Shiga-toxin producing Escherichia coli. Epidemiol Infect. 2019;147:1–10.
Centers for Disease Control and Prevention (CDC). Salmonella. 2019. https://www.cdc.gov/salmonella/general/index.html (last accessed October 19, 2022)
Eikmeier D, Medus C, Smith K. Incubation period for outbreak-associated, non-typhoidal salmonellosis cases, Minnesota, 2000-2015. Epidemiol Infect. 2018;146:423–29.
Matsui T, Suzuki S, Takahashi H, Ohyama T, Kobayashi J, Izumiya H, et al. Salmonella Enteritidis outbreak associated with a school-lunch dessert: cross-contamination and a long incubation period, Japan, 2001. Epidemiol Infect. 2004;132:873–9.
MacDougall L, Majowicz S, Dore K, Flint J, Thomas K, Kovacs S, et al. Under-reporting of infectious gastrointestinal illness in British Columbia, Canada: who is counted in Provincial communicable disease statistics? Epidemiol Infect. 2007;136:248–56.
Hong R, Baumann BM, Boudreaux ED. The emergency department for routine healthcare: race/ethnicity, socioeconomic status, and perceptual factors. J Emerg Med. 2007;32:149–58.
Acknowledgements
We wish to thank Dr. Mark LeChevallier and Dr. Tyler Radniecki for providing critical advice on the manuscript. The authors also thank Dr. Kwadwo Adu Boakye for providing GIS maps.
Funding
DH was supported in part by a US Department of Veterans Affairs Research Career Scientist award RCS 21-136. The views expressed in this manuscript are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Author information
Authors and Affiliations
Contributions
SR designed the study, acquired and analyzed the data, and wrote the manuscript; JF, LI, TA-C, PH, DH and TN-D helped design the research; and SF, AB, and PK contributed to data analyses. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The Oregon State University Institutional Review Board reviewed and approved the protocols for this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rothenberg, S.E., Furrer, J.M., Ingram, L.A. et al. Sanitary sewage overflows, boil water advisories, and emergency room and urgent care visits for gastrointestinal illness: a case-crossover study in South Carolina, USA, 2013–2017. J Expo Sci Environ Epidemiol 33, 102–110 (2023). https://doi.org/10.1038/s41370-022-00498-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41370-022-00498-7