Abstract
Background
Personal exposure to noise has been shown to be associated with concomitant increases and lagged decreases of short-term heart rate variability (HRV). It is however unknown whether this association differs between contexts defined by visited places or mobility as both exposure sources and expectations may be different between these contexts.
Method
Between July 2014 and June 2015, the RECORD MultiSensor Study collected sound level and heart rate data for 75 participants, aged 34–74 years, in their living environments for 7 days using a personal dosimeter and electrocardiography sensor on the chest. Their whereabouts were collected using a GPS receiver and a mobility survey. Short-term concomitant and lagged associations between sound level and HRV parameters were assessed within types of visited places and transport modes using mixed effects models with a random intercept for participants.
Results
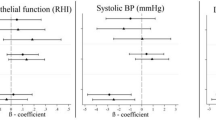
Increases in sound level were associated with a concomitant increase in all HR/HRV parameters, and delayed decreases in the overall HRV. Interactions between the sound level and the visited place/mobility context were documented. Compared with home, the concomitant association of sound level with HR and rMSSD was doubled within active and private-motorized transport modes, respectively.
Conclusions
The association of sound level with HR/HRV varies between visited places/mobility contexts. Future studies investigating these context-dependent associations in ambulatory settings will need to assess additional acoustical factors relating to the visited environments as well as non-acoustical factors impacting the perception of noise.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Basner M, Babisch W, Davis A, Brink M, Clark C, Janssen S, et al. Auditory and non-auditory effects of noise on health. Lancet 2014;383:1325–32.
Nelson DI, Nelson RY, Concha‐Barrientos M, Fingerhut M. The global burden of occupational noise‐induced hearing loss. Am J Ind Med. 2005;48:446–58.
de Kluizenaar Y, Matsui T. Recent progress in the field of non-auditory health effects of noise–trends and research needs. In: Proceedings of the 12th ICBEN congress on noise as a public health problem. Zurich; 2017. p. 1–12.
Babisch W. The noise/stress concept, risk assessment and research needs. Noise Health 2002;4:1.
El Aarbaoui T, Méline J, Brondeel R, Chaix B. Short-term association between personal exposure to noise and heart rate variability: the RECORD MultiSensor Study. Environ Pollut. 2017;231:703–11.
Schutte M, Marks A, Wenning E, Griefahn B. The development of the noise sensitivity questionnaire. Noise Health. 2007;9:15.
Chaix B, Kestens Y, Bean K, Leal C, Karusisi N, Meghiref K, et al. Cohort profile: residential and non-residential environments, individual activity spaces and cardiovascular risk factors and diseases—the RECORD Cohort Study. Int J Epidemiol. 2011;41:1283–92.
Chaix B, Kestens Y, Duncan DT, Brondeel R, Méline J, El Aarbaoui T, et al. A GPS-based methodology to analyze environment-health associations at the trip level: case-crossover analyses of built environments and walking. Am J Epidemiol. 2016;184:579–89.
Chaix B, Kestens Y, Duncan S, Merrien C, Thierry B, Pannier B, et al. Active transportation and public transportation use to achieve physical activity recommendations? A combined GPS, accelerometer, and mobility survey study. Int J Behav Nutr Phys Act. 2014;11:124.
Wolf J, Schönfelder S, Samaga U, Oliveira M, Axhausen K. Eighty weeks of global positioning system traces: approaches to enriching trip information. Transp Res Rec. 2004;1870:46–54.
Camm AJ, Malik M, Bigger J, Breithardt G, Cerutti S, Cohen RJ. et al. Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Eur Heart J. 1996;17:354–81.
Ricciardi P, Delaitre P, Lavandier C, Torchia F, Aumond P. Sound quality indicators night noise guidelines for urban places in Paris cross-validated by Milan dataEurope. J Acoustical Soc Am. 2015;138:2337–48.
Nunan D, Donovan G, Jakovljevic DG, Hodges LD, Sandercock GR, Brodie DA. Validity and reliability of short-term heart-rate variability from the Polar S810. Med Sci Sports Exerc. 2009;41:243–50.
Thayer JF, Åhs F, Fredrikson M, Sollers JJ III, Wager TD. A meta-analysis of heart rate variability and neuroimaging studies: implications for heart rate variability as a marker of stress and health. Neurosci Biobehav Rev. 2012;36:747–56.
Hill L, Siebenbrock A, Sollers J, Thayer JF. Are all measures created equal? Heart rate variability and respiration. Biomed Sci Instrum. 2009;45:71–6.
Laborde S, Mosley E, Thayer JF. Heart rate variability and cardiac vagal tone in psychophysiological research–recommendations for experiment planning, data analysis, and data reporting. Front Psychol. 2017;8:213.
Team RC. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2013.
Rodríguez-Liñares L, Méndez AJ, Lado MJ, Olivieri DN, Vila X, Gómez-Conde I. An open source tool for heart rate variability spectral analysis. Comput Methods Prog Biomed. 2011;103:39–50.
Fitzmaurice GM, Laird NM, Ware JH. Applied longitudinal analysis. Hoboken, NJ: John Wiley & Sons; 2012.
Kincaid C. Guidelines for selecting the covariance structure in mixed model analysis. In: Proceedings of the thirtieth annual SAS users group international conference. Cary, NC: SAS Institute Inc Cary NC; 2005.
Fox J, Weisberg S, Adler D, Bates D, Baud-Bovy G, Ellison S, et al. Package ‘car’. Vienna: R Foundation for Statistical Computing; 2012.
Fox J, Monette G. Generalized collinearity diagnostics. J Am Stat Assoc. 1992;87:178–83.
O’brien RM. A caution regarding rules of thumb for variance inflation factors. Qual Quant. 2007;41:673–90.
Pinheiro J, Bates D, DebRoy S, Sarkar D, Team RC. nlme: Linear and nonlinear mixed effects models. R package version 3.1-128. http://cran.r-project.org/package=nlme. 2017.
Ball R, Galecki MA. lmeSplines: Add smoothing spline modelling capability to nlme. R package version 1.1–10. http://cran.r-project.org/package=lmeSplines. 2015.
Hothorn T, Bretz F, Westfall P, Heiberger RM, Schuetzenmeister A, Scheibe S, et al. multcomp: Simultaneous Inference in General Parametric Models. R package version 1.4–8. http://cran.r-project.org/package=multcomp. 2017.
Wickham H, Chang W. ggplot2: an implementation of the grammar of graphics. R package version 2.2.1. http://cran.r-project.org/package=ggplot2. 2018.
Münzel T, Gori T, Babisch W, Basner M. Cardiovascular effects of environmental noise exposure. Eur Heart J. 2014;35:829–36.
Idrobo Ávila EH, Loaiza Correa H, Van Noorden L, Muñoz Bolaños FG, Vargas Cañas R. Different types of sounds and their relationship with the electrocardiographic signals and the cardiovascular system—review. Front Physiol. 2018;9:525.
Holand S, Girard A, Laude D, Meyer-Bisch C, Elghozi J-L. Effects of an auditory startle stimulus on blood pressure and heart rate in humans. J Hypertens. 1999;17:1893–7.
Kraus U, Schneider A, Breitner S, Hampel R, Rückerl R, Pitz M, et al. Individual daytime noise exposure during routine activities and heart rate variability in adults: a repeated measures study. Environ Health Perspect. 2013;121:607.
Buccelletti E, Gilardi E, Scaini E, Galiuto L, Persiani R, Biondi A, et al. Heart rate variability and myocardial infarction: systematic literature review and metanalysis. Eur Rev Med Pharmacol Sci. 2009;13:299–307.
Hillebrand S, Gast KB, de Mutsert R, Swenne CA, Jukema JW, Middeldorp S, et al. Heart rate variability and first cardiovascular event in populations without known cardiovascular disease: meta-analysis and dose–response meta-regression. Europace. 2013;15:742–9.
Sim CS, Sung JH, Cheon SH, Lee JM, Lee JW, Lee J. The effects of different noise types on heart rate variability in men. Yonsei Med J. 2015;56:235–43.
Oh B-S, Yeo YK, Wan FY, Wen Y, Yang Y, Lin Z. Effects of noisy sounds on human stress using ECG signals: an empirical study. In: Proceedings of the 2015 10th international conference on information, communications and signal processing (ICICS). Singapore: IEEE; 2015.
Björ B, Burström L, Karlsson M, Nilsson T, Näslund U, Wiklund U. Acute effects on heart rate variability when exposed to hand transmitted vibration and noise. Int Arch Occup Environ health. 2007;81:193–9.
Walker ED, Brammer A, Cherniack MG, Laden F, Cavallari JM. Cardiovascular and stress responses to short-term noise exposures—a panel study in healthy males. Environ Res. 2016;150:391–7.
Huang J, Deng F, Wu S, Lu H, Hao Y, Guo X. The impacts of short-term exposure to noise and traffic-related air pollution on heart rate variability in young healthy adults. J Expo Sci Environ Epidemiol. 2013;23:559.
Thayer JF, Yamamoto SS, Brosschot JF. The relationship of autonomic imbalance, heart rate variability and cardiovascular disease risk factors. Int J Cardiol. 2010;141:122–31.
Lee G-S, Chen M-L, Wang G-Y. Evoked response of heart rate variability using short-duration white noise. Auton Neurosci. 2010;155:94–7.
Cho W, Hwang S-H, Choi H. The relationship between pure-tone noise and human bio-signal response. Int J Precis Eng Manuf. 2011;12:727–31.
Chen K-H, Aksan N, Anderson SW, Grafft A, Chapleau MW. Habituation of parasympathetic-mediated heart rate responses to recurring acoustic startle. Front Psychol. 2014;5:1288.
Ising H, Michalak R. Stress effects of noise in a field experiment in comparison to reactions to short term noise exposure in the laboratory. Noise Health. 2004;6:1.
Jarrin DC, McGrath JJ, Giovanniello S, Poirier P, Lambert M. Measurement fidelity of heart rate variability signal processing: the devil is in the details. Int J Psychophysiol. 2012;86:88–97.
Heathers J, Goodwin M. LF/HF HRV: the ‘Life After Death’ of a refuted theory. http://osf.io/3pd5k. 2017.
Doberenz S, Roth WT, Wollburg E, Maslowski NI, Kim S. Methodological considerations in ambulatory skin conductance monitoring. Int J Psychophysiol. 2011;80:87–95.
Buteau S, Goldberg MS. A structured review of panel studies used to investigate associations between ambient air pollution and heart rate variability. Environ Res. 2016;148:207–47.
Jiao K, Li Z, Chen M, Wang C, Qi S. Effect of different vibration frequencies on heart rate variability and driving fatigue in healthy drivers. Int Arch Occup Environ health. 2004;77:205–12.
Young FL, Leicht AS. Short-term stability of resting heart rate variability: influence of position and gender. Appl Physiol Nutr Metab. 2011;36:210–8.
Wallenius MA. The interaction of noise stress and personal project stress on subjective health. J Environ Psychol. 2004;24:167–77.
Hautala AJ, Karjalainen J, Kiviniemi AM, Kinnunen H, Mäkikallio TH, Huikuri HV, et al. Physical activity and heart rate variability measured simultaneously during waking hours. Am J Physiol Heart Circ Physiol. 2010;298:H874–H80.
Herman Hansen B, Børtnes I, Hildebrand M, Holme I, Kolle E, Anderssen SA. Validity of the ActiGraph GT1M during walking and cycling. J Sports Sci. 2014;32:510–6.
Can A, Michel S, De Coensel B, Ribeiro C, Botteldooren D, Lavandier C. Comparison of noise indicators in an urban context. In: INTER-NOISE and NOISE-CON congress and conference proceedings. Hamburg, Germany: Institute of Noise Control Engineering; 2016.
Leventhall H. Low frequency noise and annoyance. Noise Health. 2004;6:59.
Rylander R. Physiological aspects of noise-induced stress and annoyance. J Sound Vib. 2004;277:471–8.
Westman JC, Walters JR. Noise and stress: a comprehensive approach. Environ Health Perspect. 1981;41:291.
Moskowitz DS, Young SN. Ecological momentary assessment: what it is and why it is a method of the future in clinical psychopharmacology. J Psychiatry Neurosci. 2006;31:13.
Acknowledgements
The RECORD MultiSensor Study was supported by the Ministry of Ecology (DGITM); Cerema (Centre for the Study of and Expertise on Risks, the Environment, Mobility, and Planning); INPES (National Institute for Prevention and Health Education); STIF (Ile-de-France Transportation Authority); and DRIEA (Regional and Interdepartmental Direction of Equipment and Planning) of Ile-de-France.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
El Aarbaoui, T., Chaix, B. The short-term association between exposure to noise and heart rate variability in daily locations and mobility contexts. J Expo Sci Environ Epidemiol 30, 383–393 (2020). https://doi.org/10.1038/s41370-019-0158-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41370-019-0158-x
Keywords
This article is cited by
-
Application of machine learning to predict transport modes from GPS, accelerometer, and heart rate data
International Journal of Health Geographics (2022)