Abstract
Background/Objectives
Previous studies have reported the gender-specific association between general and central obesity measures, using snapshot assessments, and mortality events. This study seeks to further explore this link by examining how the longitudinal cumulative burden and variability of obesity measures from midlife to later-life impact mortality events in the Atherosclerosis Risk in Communities (ARIC) study population, specifically in relation to gender differences.
Subjects/Methods
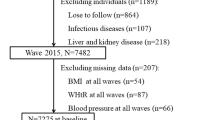
Using data from the ARIC study, a total of 7615 (4360 women) participants free of cardiovascular disease, cancer, and early mortality events were included in the data analysis. Longitudinal cumulative burden (estimated by the area under the curve (AUC) using a quadratic mixed-effects method) and variability (calculated according to average successive variability (ASV)) were considered as exposures, separately and all together. Cox proportional hazard regression models were used to estimate multivariable-adjusted standardized hazard ratios.
Results
The mean age was 62.4 and the median follow-up was 16.9 years. In men, AUCs of waist-related obesity measures, and also ASVs of all obesity measures were associated with increased all-cause mortality risk. In women, waist circumference and waist-to-height ratio AUCs were associated with increased all-cause mortality risk. Regarding cardiovascular mortality, all adiposity measures ASVs in both genders and waist-related obesity measures AUCs in men were associated with increased risk. Significant gender differences were found for the associations between cumulative and variability of waist-to-hip ratio for all-cause mortality and all adiposity measures ASVs for cardiovascular mortality risk with higher impact among men.
Conclusions
Cumulative burden and variability in general and central obesity measures were associated with higher all-cause and cardiovascular mortalities among men. In women, general obesity measures variability, as well as cumulative and variability of central adiposity measure, increased all-cause mortality risk.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Lu Y, Hajifathalian K, Ezzati M, Woodward M, Rimm EB, Danaei G, et al. Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1.8 million participants. Lancet. 2014;383:970–83.
Bray GA, Frühbeck G, Ryan DH, Wilding JP. Management of obesity. The Lancet. 2016;387:1947–56.
Ward ZJ, Willett WC, Hu FB, Pacheco LS, Long MW, Gortmaker SL. Excess mortality associated with elevated body weight in the USA by state and demographic subgroup: A modelling study. EClinicalMedicine. 2022;48:101429.
Liu B, Du Y, Wu Y, Snetselaar LG, Wallace RB, Bao W. Trends in obesity and adiposity measures by race or ethnicity among adults in the United States 2011-18: population based study. BMJ. 2021;372:n365.
Fryar CD, Kruszan-Moran D, Gu Q, Ogden CL. Mean body weight, weight, waist circumference, and body mass index among adults: United States, 1999-2000 through 2015-2016. Natl Health Stat Report. 2018;122:1–16.
Peters SAE, Muntner P, Woodward M. Sex differences in the prevalence of, and trends in, cardiovascular risk factors, treatment, and control in the United States, 2001 to 2016. Circulation. 2019;139:1025–35.
Cameron NA, Petito LC, McCabe M, Allen NB, O’brien MJ, Carnethon MR, et al. Quantifying the sex‐race/ethnicity‐specific burden of obesity on incident diabetes mellitus in the United States, 2001 to 2016: MESA and NHANES. J Am Heart Assoc. 2021;10:e018799.
Adams KF, Schatzkin A, Harris TB, Kipnis V, Mouw T, Ballard-Barbash R, et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med. 2006;355:763–78.
Feng B, Chen S, Wang X, Hu S, Zhang X, Zhang J, et al. Effect of cumulative body mass index exposure and long‐term related change on incident non‐alcoholic fatty liver disease. Liver Int. 2023;43:345–56.
Yan Y, Li S, Guo Y, Fernandez C, Bazzano L, He J, et al. Life-course cumulative burden of body mass index and blood pressure on progression of left ventricular mass and geometry in midlife: the Bogalusa Heart Study. Circul Res. 2020;126:633–43.
Cook NR, Rosner BA, Chen W, Srinivasan SR, Berenson GS. Using the area under the curve to reduce measurement error in predicting young adult blood pressure from childhood measures. Stat Med. 2004;23:3421–35.
Massey RJ, Siddiqui MK, Pearson ER, Dawed AY. Weight variability and cardiovascular outcomes: a systematic review and meta-analysis. Cardiovascul Diabetol. 2023;22:1–12.
Zou H, Yin P, Liu L, Liu W, Zhang Z, Yang Y, et al. Body-weight fluctuation was associated with increased risk for cardiovascular disease, all-cause and cardiovascular mortality: a systematic review and meta-analysis. Front Endocrinol. 2019;10:728.
Kim DH, Nam GE, Han K, Kim Y-H, Park K-Y, Hwang H-S, et al. Variabilities in weight and waist circumference and risk of myocardial infarction, stroke, and mortality: a nationwide cohort study. Endocrinol Metab. 2020;35:933.
Investigators A. The Atherosclerosis risk in COMMUNIT (ARIC) study: design and objectives. Am J Epidemiol. 1989;129:687–702.
Ferrario M, Carpenter M, Chambless L. Reliability of body fat distribution measurements. The ARIC Study baseline cohort results. Atherosclerosis Risk in Communities Study. Int J Obesity Related Metab Disord. 1995;19:449–57.
Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr. 1982;36:936–42.
Pinheiro J, Bates D, DebRoy S, Sarkar D, Heisterkamp S, Van Willigen B, et al. Package ‘nlme’. Linear and nonlinear mixed effects models, version. 2017;3.
Echouffo-Tcheugui JB, Zhao S, Brock G, Matsouaka RA, Kline D, Joseph JJ. Visit-to-visit glycemic variability and risks of cardiovascular events and all-cause mortality: the ALLHAT study. Diabetes Care. 2019;42:486–93.
Lu Z, Geurts S, Arshi B, Tilly MJ, Aribas E, van Lennep JR, et al. editors. Longitudinal anthropometric measures and risk of new-onset atrial fibrillation among community-dwelling men and women. Mayo Clinic Proceedings; 2022: Elsevier.
Yang Y, Dugué P-A, Lynch BM, Hodge AM, Karahalios A, MacInnis RJ, et al. Trajectories of body mass index in adulthood and all-cause and cause-specific mortality in the Melbourne Collaborative Cohort Study. BMJ Open. 2019;9:e030078.
Zheng H, Tumin D, Qian Z. Obesity and mortality risk: new findings from body mass index trajectories. Am J Epidemiol. 2013;178:1591–9.
Hirko KA, Kantor ED, Cohen SS, Blot WJ, Stampfer MJ, Signorello LB. Body mass index in young adulthood, obesity trajectory, and premature mortality. Am J Epidemiol. 2015;182:441–50.
Cho IJ, Chang HJ, Sung JM, Yun YM, Kim HC, Chung N. Associations of changes in body mass index with all-cause and cardiovascular mortality in healthy middle-aged adults. PLoS One. 2017;12:e0189180.
Alharbi TA, Paudel S, Gasevic D, Ryan J, Freak-Poli R, Owen AJ. The association of weight change and all-cause mortality in older adults: a systematic review and meta-analysis. Age Ageing. 2021;50:697–704.
Wilsgaard T, Jacobsen BK, Mathiesen EB, Njølstad I. Weight loss and mortality: a gender-specific analysis of the Tromsø study. Gend Med. 2009;6:575–86.
Tamakoshi K, Yatsuya H, Kondo T, Ishikawa M, Zhang H, Murata C, et al. Long-term body weight variability is associated with elevated C-reactive protein independent of current body mass index among Japanese men. Int J Obesity. 2003;27:1059–65.
Strohacker K, McFarlin BK. Influence of obesity, physical inactivity, and weight cycling on chronic inflammation. Front Biosci (Elite edition). 2010;2:98–104.
Patsouras MD, Vlachoyiannopoulos PG. Evidence of epigenetic alterations in thrombosis and coagulation: a systematic review. J Autoimmun. 2019;104:102347.
Hunt BJ, editor Hemostasis at extremes of body weight. Seminars in Thrombosis and Hemostasis; 2018: Thieme Medical Publishers.
McGee DL, Collaboration DP. Body mass index and mortality: a meta-analysis based on person-level data from twenty-six observational studies. Annals of epidemiology. 2005;15:87–97.
Yatsuya H, Tamakoshi K, Yoshida T, Hori Y, Zhang H, Ishikawa M, et al. Association between weight fluctuation and fasting insulin concentration in Japanese men. Int J Obes Relat Metab Disord. 2003;27:478–83.
Anastasiou CA, Yannakoulia M, Pirogianni V, Rapti G, Sidossis LS, Kavouras SA. Fitness and weight cycling in relation to body fat and insulin sensitivity in normal-weight young women. J Am Dietetic Assoc. 2010;110:280–4.
French SA, Jeffery RW, Folsom AR, Williamson DF, Byers T. Relation of weight variability and intentionality of weight loss to disease history and health-related variables in a population-based sample of women aged 55–69 years. Am J Epidemiol. 1995;142:1306–14.
Waring ME, Eaton CB, Lasater TM, Lapane KL. Incident diabetes in relation to weight patterns during middle age. Am J Epidemiol. 2010;171:550–6.
Field AE, Manson JE, Laird N, Williamson DF, Willett WC, Colditz GA. Weight cycling and the risk of developing type 2 diabetes among adult women in the United States. Obesity Res. 2004;12:267–74.
Wing RR, Jeffery RW, Hellerstedt WL. A prospective study of effects of weight cycling on cardiovascular risk factors. Arch Internal Med. 1995;155:1416–22.
Olson MB, Kelsey SF, Bittner V, Reis SE, Reichek N, Handberg EM, et al. Weight cycling and high-density lipoprotein cholesterol in women: evidence of an adverse effect: a report from the NHLBI-sponsored WISE study. J Am College of Cardiol. 2000;36:1565–71.
Cereda E, Malavazos AE, Caccialanza R, Rondanelli M, Fatati G, Barichella M. Weight cycling is associated with body weight excess and abdominal fat accumulation: a cross-sectional study. Clin Nutr. 2011;30:718–23.
Wallner S, Luschnigg N, Schnedl W, Lahousen T, Sudi K, Crailsheim K, et al. Body fat distribution of overweight females with a history of weight cycling. Int J Obesity. 2004;28:1143–8.
Pankow JS, Tang W, Pankratz N, Guan W, Weng L-C, Cushman M, et al. Identification of genetic variants linking protein C and lipoprotein metabolism: the ARIC study (Atherosclerosis Risk in Communities). Arteriosclerosis Thrombosis Vascular Biol. 2017;37:589–97.
Gaillard R, Steegers EA, Tiemeier H, Hofman A, Jaddoe VW. Placental vascular dysfunction, fetal and childhood growth, and cardiovascular development: the generation R study. Circulation. 2013;128:2202–10.
Heise L, Greene ME, Opper N, Stavropoulou M, Harper C, Nascimento M, et al. Gender inequality and restrictive gender norms: framing the challenges to health. The Lancet. 2019;393:2440–54.
Stringhini S, Carmeli C, Jokela M, Avendaño M, Muennig P, Guida F, et al. Socioeconomic status and the 25× 25 risk factors as determinants of premature mortality: a multicohort study and meta-analysis of 1· 7 million men and women. The Lancet. 2017;389:1229–37.
Dwivedi AK, Vishwakarma D, Dubey P, Reddy SY. Air pollution and the heart: updated evidence from meta-analysis studies. Curr Cardiol Rep. 2022;24:1811–35.
Dubey P, Reddy SY, Singh V, Shi T, Coltharp M, Clegg D, et al. Association of exposure to phthalate metabolites with sex hormones, obesity, and metabolic syndrome in US women. JAMA Network Open. 2022;5:e2233088-e.
Kander MC, Cui Y, Liu Z. Gender difference in oxidative stress: a new look at the mechanisms for cardiovascular diseases. J Cellular Mol Med. 2017;21:1024–32.
Han X, Stevens J, Truesdale KP, Bradshaw PT, Kucharska-Newton A, Prizment AE, et al. Body mass index at early adulthood, subsequent weight change and cancer incidence and mortality. Int J Cancer. 2014;135:2900–9.
Argyrakopoulou G, Dalamaga M, Spyrou N, Kokkinos A. Gender differences in obesity-related cancers. Curr Obesity Rep. 2021;10:100–15.
Harrington M, Gibson S, Cottrell RC. A review and meta-analysis of the effect of weight loss on all-cause mortality risk. Nutr Res Rev. 2009;22:93–108.
Locher JL, Roth DL, Ritchie CS, Cox K, Sawyer P, Bodner EV, et al. Body mass index, weight loss, and mortality in community-dwelling older adults. J Gerontol A Biol Sci Med Sci. 2007;62:1389–92.
Kaze AD, Santhanam P, Erqou S, Ahima RS, Bertoni AG, Echouffo-Tcheugui JB. Body weight variability and risk of cardiovascular outcomes and death in the context of weight loss intervention among patients with type 2 diabetes. JAMA Netw Open. 2022;5:e220055-e.
St-Onge MP, Gallagher D. Body composition changes with aging: the cause or the result of alterations in metabolic rate and macronutrient oxidation? Nutrition. 2010;26:152–5.
Acknowledgements
We thank the participants ARIC study and the Biologic Specimen and Data Repository Information Coordinating Center (BioLINCC) website staff for their contributions.
Author information
Authors and Affiliations
Contributions
FH and KK were responsible for the study conceptualization and design, analysis of demographic data, interpretation of results, and preparation of the manuscript. KK was responsible for analytic design and data analysis. KK, FH, SA, DK, and DM were responsible for the conceptualization of the study. All listed authors reviewed the manuscript and agree to be accountable for all aspects of this work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kohansal, K., Afaghi, S., Khalili, D. et al. Gender differences in midlife to later-life cumulative burden and variability of obesity measures and risk of all-cause and cause-specific mortality. Int J Obes 48, 495–502 (2024). https://doi.org/10.1038/s41366-023-01440-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-023-01440-z