Abstract
Background
Recent studies suggest that tirzepatide, a dual glucose-dependent insulinotropic-peptide (GIP) and glucagon-like peptide-1 receptor agonist (GLP-1 RA), has significant weight loss effects. This systematic review and meta-analysis aims to assess the efficacy and safety of tirzepatide for weight loss in patients with overweight or obesity.
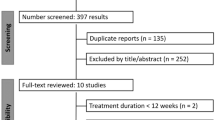
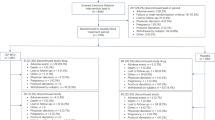
Methods
Medline, Embase and Cochrane CENTRAL were searched for randomized controlled trials (RCTs) on tirzepatide’s weight loss efficacy for these patients. A single arm meta-analysis of proportions estimated primary outcomes, ≥5%, ≥10%, and ≥15% weight loss, and adverse events (AEs); while meta-analysis of means estimated secondary outcomes. Comparative meta-analysis was conducted between tirzepatide and control arms where mean differences and odds ratios were estimated for continuous and dichotomous outcomes respectively.
Results
RCTs included in this study revealed that among 5800 patients, 78.22% (95% CI: 72.15% to 83.73%), 55.60% (95% CI: 46.54% to 64.47%), 32.28% (95% CI: 23.17% to 42.12%) achieved ≥5%, ≥10%, and ≥15% weight loss, respectively. Tirzepatide 5 mg demonstrated weight loss superiority relative to placebo (MD: −12.47 kg, 95% CI: −13.94 kg to −11.00 kg) and semaglutide (n = 1409, MD: −1.90 kg, 95% CI: −2.97 kg to −0.83 kg) with dose-dependent increase for 10 mg and 15 mg doses. The comparison between tirzepatide and semaglutide was examined in the SURPASS-2 trial that was included in this systematic review. For AEs, there was increase odds of experiencing gastrointestinal AEs with tirzepatide compared to placebo, but no significant difference with semaglutide.
Conclusion
Tirzepatide has significant potential as a weight loss drug in patients with overweight and obesity, with little increase in AEs compared to other weight loss drugs. With its ability to concurrently target multiple aspects of metabolic syndrome, it should be considered as the next helm of weight loss therapies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
All articles in this manuscript are available from Medline and Embase.
References
Chong B, Kong G, Shankar K, Chew HSJ, Lin C, Goh R, et al. The global syndemic of metabolic diseases in the young adult population: a consortium of trends and projections from the Global Burden of Disease 2000–2019. Metabolism. 2023;141:155402. https://doi.org/10.1016/j.metabol.2023.155402.
Chew NWS, Ng CH, Tan DJH, Kong G, Lin C, Chin YH, et al. The global burden of metabolic disease: Data from 2000 to 2019. Cell Metab. 2023;35:414–28.e3. https://doi.org/10.1016/j.cmet.2023.02.003.
Organisation WH. Obesity and overweight fact sheet. World Health Organisation. Accessed 01/05/2022, 2022. https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight.
Kinlen D, Cody D, O’Shea D. Complications of obesity. QJM. 2018;111:437–43. https://doi.org/10.1093/qjmed/hcx152.
Garvey WT, Mechanick JI, Brett EM, Garber AJ, Hurley DL, Jastreboff AM, et al. American association of clinical endocrinologists and American College of Endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity. Endocr Pract. 2016;22:1–203. https://doi.org/10.4158/EP161365.GL.
Muthiah MD, Cheng Han N, Sanyal AJ. A clinical overview of non-alcoholic fatty liver disease: a guide to diagnosis, the clinical features, and complications—what the non-specialist needs to know. Diabetes Obes Metab. 2022;24:3–14. https://doi.org/10.1111/dom.14521.
Chew NWS, Ng CH, Muthiah MD, Sanyal AJ. Comprehensive review and updates on holistic approach towards non-alcoholic fatty liver disease management with cardiovascular disease. Curr Atheroscler Rep. 2022; https://doi.org/10.1007/s11883-022-01027-5.
Avila C, Holloway AC, Hahn MK, Morrison KM, Restivo M, Anglin R, et al. An overview of links between obesity and mental health. Curr Obes Rep. 2015;4:303–10.
Nyberg ST, Batty GD, Pentti J, Virtanen M, Alfredsson L, Fransson EI, et al. Obesity and loss of disease-free years owing to major non-communicable diseases: a multicohort study. Lancet Public Health. 2018;3:e490–7.
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–60.
de la Iglesia R, Loria-Kohen V, Zulet MA, Martinez JA, Reglero G, de Molina AR. Dietary strategies implicated in the prevention and treatment of metabolic syndrome. Int J Mol Sci. 2016;17. https://doi.org/10.3390/ijms17111877.
Lin C, Yeong TJJ, Lim WH, Ng CH, Chun EY, Chin YH, et al. Comparison of mechanistic pathways of bariatric surgery in patients with diabetes mellitus: a Bayesian network meta-analysis. Obesity (Silver Spring). 2022;30:1380–90. https://doi.org/10.1002/oby.23453.
Frías JP, Davies MJ, Rosenstock J, Manghi FCP, Lando LF, Bergman BK, et al. Tirzepatide versus semaglutide once weekly in patients with type 2 diabetes. Clinical Trial, Phase III; Comparative Study; Equivalence Trial; Journal Article; Multicenter Study; Randomized Controlled Trial; Research Support, Non‐U.S. Gov’t. N Engl J Med. 2021;385:503–15. https://doi.org/10.1056/NEJMoa2107519.
Karagiannis T, Avgerinos I, Liakos A, Del Prato S, Matthews DR, Tsapas A, et al. Management of type 2 diabetes with the dual GIP/GLP-1 receptor agonist tirzepatide: a systematic review and meta-analysis. Diabetologia. 2022;65:1251–61. https://doi.org/10.1007/s00125-022-05715-4.
Bhagavathula AS, Vidyasagar K, Tesfaye W. Efficacy and safety of tirzepatide in patients with type 2 diabetes mellitus: a systematic review and meta-analysis of randomized phase II/III trials. Pharmaceuticals (Basel, Switzerland). 2021;14. https://doi.org/10.3390/ph14100991.
Jung HN, Jung CH. The upcoming weekly tides (Semaglutide vs. Tirzepatide) against obesity: STEP or SURPASS? Review. J Obes Metab Syndr. 2022;31:28–36. https://doi.org/10.7570/JOMES22012.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71.
Kolkailah AA, Doukky R, Pelletier MP, Volgman AS, Kaneko T, Nabhan AF. Transcatheter aortic valve implantation versus surgical aortic valve replacement for severe aortic stenosis in people with low surgical risk. Cochrane Database Syst Rev. 2019;12:Cd013319. https://doi.org/10.1002/14651858.CD013319.pub2.
Liao YB, Li YJ, Jun-Li L, Zhao ZG, Wei X, Tsauo JY, et al. Incidence, predictors and outcome of prosthesis-patient mismatch after transcatheter aortic valve replacement: a systematic review and meta-analysis. Sci Rep. 2017;7:15014. https://doi.org/10.1038/s41598-017-15396-4.
Consultation WHOE. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. https://doi.org/10.1016/S0140-6736(03)15268-3.
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. https://doi.org/10.1186/1471-2288-14-135.
Clopper CJ, Pearson ES. The use of confidence or fiducial limits illustrated in the case of the binomial. Biometrika. 1934;26:404–13. https://doi.org/10.2307/2331986.
Schwarzer G, Chemaitelly H, Abu-Raddad LJ, Rucker G. Seriously misleading results using inverse of Freeman-Tukey double arcsine transformation in meta-analysis of single proportions. Res Synth Methods. 2019;10:476–83. https://doi.org/10.1002/jrsm.1348.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88. https://doi.org/10.1016/0197-2456(86)90046-2.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Bmj. 2003;327:557–60. https://doi.org/10.1136/bmj.327.7414.557.
Deeks JJ, Higgins JPT, Altman DG. Analysing data and undertaking meta-analyses. Cochrane Handbook for Systematic Reviews of Interventions. 2008:243–96. https://training.cochrane.org/handbook/current/chapter-10.
Harrer M, Cuijpers P, Furukawa TA, Ebert DD. Doing Meta-Analysis With R: A Hands-On Guide. 1st ed. Chapman & Hall/CRC Press; 2021.
Collaboration TC. Recommendations on testing for funnel plot asymmetry. Accessed 17 August 2022, 2022. https://handbook-5-1.cochrane.org/chapter_10/10_4_3_1_recommendations_on_testing_for_funnel_plot_asymmetry.htm.
Sterne JAC, Savovic J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. https://doi.org/10.1136/bmj.l4898.
Jastreboff AM, Aronne LJ, Ahmad NN, Wharton S, Connery L, Alves B, et al. Tirzepatide once weekly for the treatment of obesity. Journal: Article in Press. N Engl J Med. 2022; https://doi.org/10.1056/NEJMoa2206038.
Ludvik B, Giorgino F, Jodar E, Frias JP, Lando LF.Brown K, et al. Once-weekly tirzepatide versus once-daily insulin degludec as add-on to metformin with or without SGLT2 inhibitors in patients with type 2 diabetes (SURPASS-3): a randomised, open-label, parallel-group, phase 3 trial. Lancet (London, England). 2021;398:583–98. https://doi.org/10.1016/S0140-6736(21)01443-4. Comment in: Lancet. 2021; 398:560–561. PMID: 34370968 https://www.ncbi.nlm.nih.gov/pubmed/34370968.
Del Prato S, Kahn SE, Pavo I, Weerakkody GJ, Yang Z, Doupis J, et al. Tirzepatide versus insulin glargine in type 2 diabetes and increased cardiovascular risk (SURPASS-4): a randomised, open-label, parallel-group, multicentre, phase 3 trial. Journal Article; Clinical Trial Protocol. Lancet. 2021;398:1811–24. https://doi.org/10.1016/S0140-6736(21)02188-7.
Coskun T, Sloop KW, Loghin C, Alsina-Fernandez J, Urva S, Bokvist KB, et al. LY3298176, a novel dual GIP and GLP-1 receptor agonist for the treatment of type 2 diabetes mellitus: from discovery to clinical proof of concept. Mol Metab. 2018;18:3–14. https://doi.org/10.1016/j.molmet.2018.09.009.
Kadowaki T, Chin R, Ozeki A, Imaoka T, Ogawa Y. Safety and efficacy of tirzepatide as an add-on to single oral antihyperglycaemic medication in patients with type 2 diabetes in Japan (SURPASS J-combo): a multicentre, randomised, open-label, parallel-group, phase 3 trial. Lancet Diabetes Endocr. 2022;10:634–44. https://doi.org/10.1016/s2213-8587(22)00187-5.
Heise T, Mari A, DeVries JH, Urva S, Li J, Pratt EJ, et al. Effects of subcutaneous tirzepatide versus placebo or semaglutide on pancreatic islet function and insulin sensitivity in adults with type 2 diabetes: a multicentre, randomised, double-blind, parallel-arm, phase 1 clinical trial. Clinical Trial, Phase I; Journal Article; Multicenter Study; Randomized Controlled Trial; Research Support, Non‐U.S. Gov’t. Lancet Diabetes Endocrinol. 2022;10:418–29. https://doi.org/10.1016/S2213-8587(22)00085-7.
O’Neil PM, Birkenfeld AL, McGowan B, Mosenzon O, Pedersen SD, Wharton S, et al. Efficacy and safety of semaglutide compared with liraglutide and placebo for weight loss in patients with obesity: a randomised, double-blind, placebo and active controlled, dose-ranging, phase 2 trial. Lancet. 2018;392:637–49. https://doi.org/10.1016/S0140-6736(18)31773-2.
Min T, Bain SC. The role of tirzepatide, dual GIP and GLP-1 receptor agonist, in the management of type 2 diabetes: the SURPASS clinical trials. Rev Diabetes Ther. 2021;12:143–57. https://doi.org/10.1007/s13300-020-00981-0.
Frias JP, Nauck MA, Van J, Kutner ME, Cui X, Benson C, et al. Efficacy and safety of LY3298176, a novel dual GIP and GLP-1 receptor agonist, in patients with type 2 diabetes: a randomised, placebo-controlled and active comparator-controlled phase 2 trial. Lancet. 2018;392:2180–93. https://doi.org/10.1016/s0140-6736(18)32260-8.
Chin YH, Ng CH, Chew NW, Kong G, Lim WH, Tan DJH, et al. The placebo response rate and nocebo events in obesity pharmacological trials. A systematic review and meta-analysis. EClinicalMedicine. 2022;54:101685. https://doi.org/10.1016/j.eclinm.2022.101685.
Engin A. The definition and prevalence of obesity and metabolic syndrome. Adv Exp Med Biol. 2017;960:1–17. https://doi.org/10.1007/978-3-319-48382-5_1.
Muthiah M, Ng CH, Chan KE, Fu CE, Lim WH, Tan DJH, et al. Type 2 diabetes mellitus in metabolic-associated fatty liver disease vs. type 2 diabetes mellitus non-alcoholic fatty liver disease: a longitudinal cohort analysis. Ann Hepatol. 2023;28:100762. https://doi.org/10.1016/j.aohep.2022.100762.
Bramante CT, Raatz S, Bomberg EM, Oberle MM, Ryder JR. Cardiovascular risks and benefits of medications used for weight loss. Front Endocrinol (Lausanne). 2019;10:883. https://doi.org/10.3389/fendo.2019.00883.
Salari N, Jafari S, Darvishi N, Valipour E, Mohammadi M, Mansouri K, et al. The best drug supplement for obesity treatment: a systematic review and network meta-analysis. Diabetol Metab Syndr. 2021;13:110. https://doi.org/10.1186/s13098-021-00733-5.
Vosoughi K, Atieh J, Khanna L, Khoshbin K, Prokop LJ, Davitkov P, et al. Association of glucagon-like peptide 1 analogs and agonists administered for obesity with weight loss and adverse events: a systematic review and network meta-analysis. EClinicalMedicine. 2021;42:101213. https://doi.org/10.1016/j.eclinm.2021.101213.
Cacciottolo TM, Evans K. Research in brief: effective pharmacotherapy for the management of obesity. Clin Med (Lond). 2021;21:e517–8. https://doi.org/10.7861/clinmed.2021-0253.
Fornes A, Huff J, Pritchard RI, Godfrey M. Once-weekly semaglutide for weight management: a clinical review. J Pharm Technol. 2022;38:239–46. https://doi.org/10.1177/87551225221092681.
Ng CH, Lin SY, Chin YH, Lee MH, Syn N, Goh XL, et al. Antidiabetic medications for type 2 diabetics with nonalcoholic fatty liver disease: evidence from a network meta-analysis of randomized controlled trials. Endocr Pract. 2022;28:223–30. https://doi.org/10.1016/j.eprac.2021.09.013.
Quek J, Chan KE, Wong ZY, Tan C, Tan B, Lim WH, et al. Global prevalence of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in the overweight and obese population: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2023;8:20–30. https://doi.org/10.1016/s2468-1253(22)00317-x.
Le MH, Yeo YH, Zou B, Barnet S, Henry L, Cheung R, et al. Forecasted 2040 global prevalence of nonalcoholic fatty liver disease using hierarchical bayesian approach. Clin Mol Hepatol. 2022;28:841–50. https://doi.org/10.3350/cmh.2022.0239.
Kang SH, Cho Y, Jeong SW, Kim SU, Lee JW, Korean NSG. From nonalcoholic fatty liver disease to metabolic-associated fatty liver disease: big wave or ripple? Clin Mol Hepatol. 2021;27:257–69. https://doi.org/10.3350/cmh.2021.0067.
Paschos P, Paletas K. Non alcoholic fatty liver disease and metabolic syndrome. Hippokratia. 2009;13:9–19.
Gastaldelli A, Cusi K, Fernandez Lando L, Bray R, Brouwers B, Rodriguez A. Effect of tirzepatide versus insulin degludec on liver fat content and abdominal adipose tissue in people with type 2 diabetes (SURPASS-3 MRI): a substudy of the randomised, open-label, parallel-group, phase 3 SURPASS-3 trial. Lancet Diabetes Endocrinol. 2022;10:393–406. https://doi.org/10.1016/S2213-8587(22)00070-5.
Roborel de Climens A, Pain E, Boss A, Shaunik A. Understanding reasons for treatment discontinuation, attitudes and education needs among people who discontinue type 2 diabetes treatment: results from an online patient survey in the USA and UK. Diabetes Ther. 2020;11:1873–81. https://doi.org/10.1007/s13300-020-00843-9.
Sattar N, McGuire DK, Pavo I, Weerakkody GJ, Nishiyama H, Wiese RJ, et al. Tirzepatide cardiovascular event risk assessment: a pre-specified meta-analysis. Nat Med. 2022;28:591–8. https://doi.org/10.1038/s41591-022-01707-4.
Kong G, Chin YH, Chong B, Goh RSJ, Lim OZH, Ng CH, et al. Higher mortality in acute coronary syndrome patients without standard modifiable risk factors: results from a global meta-analysis of 1,285,722 patients. Int J Cardiol. 2023;371:432–40. https://doi.org/10.1016/j.ijcard.2022.09.062.
Vorsanger MH, Subramanyam P, Weintraub HS, Lamm SH, Underberg JA, Gianos E, et al. Cardiovascular Effects of the New Weight Loss Agents. J Am Coll Cardiol. 2016;68:849–59. https://doi.org/10.1016/j.jacc.2016.06.007.
Gerstein HC, Colhoun HM, Dagenais GR, Diaz R, Lakshmanan M, Pais P, et al. Dulaglutide and cardiovascular outcomes in type 2 diabetes (REWIND): a double-blind, randomised placebo-controlled trial. Lancet. 2019;394:121–30. https://doi.org/10.1016/S0140-6736(19)31149-3.
Nct. A study of tirzepatide (LY3298176) compared with dulaglutide on major cardiovascular events in participants with type 2 diabetes (SURPASS-CVOT). https://www.clinicaltrials.gov/ct2/show/NCT04255433.
A study of tirzepatide (LY3298176) in participants with heart failure with preserved ejection fraction and obesity (SUMMIT). https://ClinicalTrials.gov/show/NCT04847557.
Willoughby D, Hewlings S, Kalman D. Body composition changes in weight loss: strategies and supplementation for maintaining lean body mass, a brief review. Nutrients. 2018;10. https://doi.org/10.3390/nu10121876.
Acknowledgements
All authors have made substantial contributions to all the following: (1) the conception and design of the study, or acquisition of data, or analysis and interpretation of data, (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted. No writing assistance was obtained in the preparation of the manuscript. The manuscript, including related data, figures and tables has not been previously published and that the manuscript is not under consideration elsewhere.
Author information
Authors and Affiliations
Contributions
Conceptualization—YHC, NWSC, MDM, MN, CHN. Data curation—BT, X-HP, YHC. Formal analysis—YHC, RSJG, CL, VVA, ECZL. Supervision—DYY, MYC, CMK, AM, MDM, MN, CHN, NWSC. Validation—YHC, NWSC, CHN, NWSC. Writing, original draft – BT, X-HP, YHC. Writing, review, and editing—BT, X-HP, YHC, HSJC, RSJG, CL, VVA, ECZL, KEC, GK, CEYO, HCC, DYY, MYC, CMK, AM, MDM, MN, CHN, NWSC. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Corresponding authors
Ethics declarations
Competing interests
MYC: Speaker’s fees and research grants Astra Zeneca, Abbott Technologies and Boston Scientific. MN: MN has been on the advisory board for 89BIO, Gilead, Intercept, Pfizer, Novo Nordisk, Blade, EchoSens, Fractyl, Terns, Siemens and Roche diagnostic; he has received research support from Allergan, BMS, Gilead, Galmed, Galectin, Genfit, Conatus, Enanta, Madrigal, Novartis, Pfizer, Shire, Viking and Zydus; he is a minor shareholder or has stocks in Anaetos, Rivus Pharma and Viking. All other authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tan, B., Pan, XH., Chew, H.S.J. et al. Efficacy and safety of tirzepatide for treatment of overweight or obesity. A systematic review and meta-analysis. Int J Obes 47, 677–685 (2023). https://doi.org/10.1038/s41366-023-01321-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-023-01321-5