Abstract
Background
The structured days hypothesis posits that ‘structured days’ (i.e., days with pre-planned, segmented, and adult-supervised environments) reduce youth obesogenic behaviors. Structured days may be especially important for adolescents’, as adolescence (12–19 years) is a period of developmental milestones and increased autonomy. Therefore, the objective of this systematic review and meta-analysis is to evaluate the relationship between structured days and adolescents’ obesogenic behaviors (i.e., physical activity, diet, screen time, and/or sleep).
Methods
From February to April of 2020, four databases (i.e., Embase, PubMed, Web of Science, and PsychINfo) were searched for cross-sectional, longitudinal, and intervention (i.e., baseline data only) studies reporting obesogenic behaviors on more structured versus less structured days (i.e., weekday versus weekend or school year versus summer/holiday).
Results
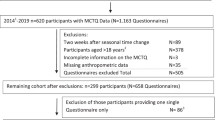
A total of 42,878 unique titles and abstracts were screened with 2767 full-text articles retrieved. After review of full-text articles, 296 studies were identified (sleep k = 147, physical activity k = 88, screen time k = 81, diet k = 8). Most studies were conducted in North America, Europe & Central Asia, or East Asia & the Pacific used self-report measures and compared school days to weekend days. Meta-analyses indicated that adolescents’ physical activity (standardized mean difference [SMD] = −0.25 [95%CI − 0.48, −0.03]) and screen time (SMD = −0.48 [95%CI − 0.66, −0.29]) were less healthy on less structured days. Differences did not reach statistical significance for sleep (SMD = −0.23 [95%CI − 0.48, 0.02]) and diet (SMD = −0.13 [95%CI − 0.77, 0.51]), however, sleep timing (SMD = −1.05 [95%CI − 1.31, −0.79]) and diet quantity (SMD = −0.29 [95%CI − 0.35, −0.23]) were less healthy on less structured days. The review identified studies with large heterogeneity.
Conclusions
Findings indicate that adolescents’ physical activity, screen time, sleep timing, and diet quantity are less healthy on less structured days. Interventions for adolescents to prevent and treat obesity may be more successful if they are designed to target times that are less structured.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others

References
Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity among adults and youth: United States, 2015–2016. Hyattsville, MD; 2017. https://stacks.cdc.gov/view/cdc/49223, cited October 7th, 2021.
Cote AT, Harris KC, Panagiotopoulos C, Sandor GG, Devlin AM. Childhood obesity and cardiovascular dysfunction. JACC. 2013;62:1309–19.
Bacha F, Gidding SS. Cardiac abnormalities in youth with obesity and type 2 diabetes. Curr Diab Rep. 2016;16:1–9.
Mohanan S, Tapp H, McWilliams A, Dulin M. Obesity and asthma: pathophysiology and implications for diagnosis and management in primary care. Exp Biol Med. 2014;239:1531–40.
Narang I, Mathew JL. Childhood obesity and obstructive sleep apnea. J Nutr Metab. 2012;2012:1–8.
Pollock NK. Childhood obesity, bone development, and cardiometabolic risk factors. Mol Cell Endocrinol. 2015;410:52–63.
Koplan JP, Liverman CT, Kraak VI. Preventing childhood obesity: health in the balance: executive summary. J Am Diet Assoc. 2005;105:131–8.
Bauer KW, Marcus MD, Larson N, Neumark-Sztainer D. Socioenvironmental, personal, and behavioral correlates of severe obesity among an ethnically/racially diverse sample of US adolescents. Child Obes. 2017;13:470–8.
Hall KD, Heymsfield SB, Kemnitz JW, Klein S, Schoeller DA, Speakman JR. Energy balance and its components: implications for body weight regulation. Am J Clin Nutr. 2012;95:989–94.
Economos CD, Hyatt RR, Must A, Goldberg JP, Kuder J, Naumova EN, et al. Shape up somerville two-year results: a community-based environmental change intervention sustains weight reduction in children. Prev Med. 2013;57:322–7.
Williams JA, Zimmerman FJ, Bell JF. Norms and trends of sleep time among US children and adolescents. JAMA Pediatr. 2013;167:55–60.
Falbe J, Willett WC, Rosner B, Gortmaker SL, Sonneville KR, Field AE. Longitudinal relations of television, electronic games, and digital versatile discs with changes in diet in adolescents. Am J Clin Nutr. 2014;100:1173–81.
Rich C, Griffiths LJ, Dezateux C. Seasonal variation in accelerometer-determined sedentary behaviour and physical activity in children: a review. Int J Behav Nutr Phys Act. 2012;9:49.
Caldwell LL, Smith EA. Leisure as a context for youth development and delinquency prevention. Aust N Z J Criminol. 2006;39:398–418.
Brazendale K, Beets MW, Weaver RG, Pate RR, Turner-McGrievy GM, Kaczynski AT, et al. Understanding differences between summer vs. school obesogenic behaviors of children: the structured days hypothesis. Int J Behav Nutr Phys Act. 2017;14:100.
Brazendale K, Beets MW, Turner-McGrievy GM, Kaczynski AT, Pate RR, Weaver RG. Children’s obesogenic behaviors during summer versus school: a within-person comparison. J School Health. 2018;88:886–92.
Hopkins LC, Tiba S, Westrick M, Gunther C. The diet quality of a sample of predominantly racial minority children from low-income households is lower during the summer vs school year: results from the project summer weight and environmental assessment trial substudy. J Acad Nutr Diet. 2021;121:112–20.
Hunt ET, von Klinggraeff L, Jones A, Burkart S, Dugger R, Armstrong B, et al. Differences in the proportion of children meeting behavior guidelines between summer and school by socioeconomic status and race. Obes Sci Pract. 2021;2021:1–8.
Weaver R, Armstrong B, Hunt E, Beets M, Brazendale K, Dugger R, et al. The impact of summer vacation on children’s obesogenic behaviors and body mass index: a natural experiment. Int J Behav Nutr Phys Act. 2020;2020:153.
Dugger R, Brazendale K, Hunt ET, Moore JB, Turner-Mcgrievy G, Vogler K, et al. The impact of summer programming on the obesogenic behaviors of children: behavioral outcomes from a quasi-experimental pilot trial. Pilot Feasibility Stud. 2020;6:1–15.
Brazendale K, Rayan S, Eisenstein D, Blankenship M, Rey A, Garcia J. et al. Obesogenic behaviors of rural children on school and nonschool days. Child Obes. 2021;17:483–492.
Brazendale K, Brazendale AB, Garcia JM, Monroe CM, Weaver RG, Beets MW brief report: obesogenic behaviors of children with developmental disabilities during summer. J Autism Dev Disord. 2020.
Moreno JP, Johnston CA, Woehler D. Changes in weight over the school year and summer vacation: results of a 5‐year longitudinal study. J Sch Health. 2013;83:473–7.
von Hippel PT, Workman J. From kindergarten through second grade, US children’s obesity prevalence grows only during summer vacations. Obesity. 2016;24:2296–300.
Franckle R, Adler R, Davison K. Accelerated weight gain among children during summer versus school year and related racial/ethnic disparities: a systematic review. Prev Chronic Dis. 2014;11:1–10.
Trzesniewski KH, Donnellan MB, Moffitt TE, Robins RW, Poulton R, Caspi A. Low self-esteem during adolescence predicts poor health, criminal behavior, and limited economic prospects during adulthood. Dev Psychol. 2006;42:381.
van Sluijs EM, Ekelund U, Crochemore-Silva I, Guthold R, Ha A, Lubans D, et al. Physical activity behaviours in adolescence: current evidence and opportunities for intervention. The Lancet. 2021;398:429–442.
Azzopardi PS, Hearps SJ, Francis KL, Kennedy EC, Mokdad AH, Kassebaum NJ, et al. Progress in adolescent health and wellbeing: tracking 12 headline indicators for 195 countries and territories, 1990–2016. The Lancet. 2019;393:1101–18.
Guthold R, Stevens GA, Riley LM, Bull FC. Global trends in insufficient physical activity among adolescents: a pooled analysis of 298 population-based surveys with 1· 6 million participants. Lancet Child Adolesc Health. 2020;4:23–35.
Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40:181.
Yang L, Cao C, Kantor ED, Nguyen LH, Zheng X, Park Y, et al. Trends in sedentary behavior among the US population, 2001-2016. JAMA. 2019;321:1587–97.
Nelson MC, Neumark-Stzainer D, Hannan PJ, Sirard JR, Story M. Longitudinal and secular trends in physical activity and sedentary behavior during adolescence. Pediatrics. 2006;118:e1627–e34.
Albani V, Butler LT, Traill WB, Kennedy OB. Fruit and vegetable intake: change with age across childhood and adolescence. Br J Nutr. 2017;117:759–65.
Craigie AM, Lake AA, Kelly SA, Adamson AJ, Mathers JC. Tracking of obesity-related behaviours from childhood to adulthood: a systematic review. Maturitas. 2011;70:266–84.
Movassagh E, Baxter-Jones A, Kontulainen S, Whiting S, Vatanparast H. Tracking dietary patterns over 20 years from childhood through adolescence into young adulthood: the Saskatchewan pediatric bone mineral accrual study. Nutrients. 2017;9:990.
Neumark-Sztainer D, Wall M, Larson NI, Eisenberg ME, Loth K. Dieting and disordered eating behaviors from adolescence to young adulthood: findings from a 10-year longitudinal study. J Am Diet Ass. 2011;111:1004–11.
Fredriksen K, Rhodes J, Reddy R, Way N. Sleepless in Chicago: tracking the effects of adolescent sleep loss during the middle school years. Child Dev. 2004;75:84–95.
Scholle S, Beyer U, Bernhard M, Eichholz S, Erler T, Graneß P, et al. Normative values of polysomnographic parameters in childhood and adolescence: quantitative sleep parameters. Sleep Med. 2011;12:542–9.
Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc Sci Med. 2010;71:1027–36.
Olds TS, Maher CA, Matricciani L. Sleep duration or bedtime? Exploring the relationship between sleep habits and weight status and activity patterns. Sleep. 2011;34:1299–307.
Patton GC, Sawyer SM, Santelli JS, Ross DA, Afifi R, Allen NB, et al. Our future: a Lancet commission on adolescent health and wellbeing. The Lancet. 2016;387:2423–78.
Arnett JJ, Žukauskienė R, Sugimura K. The new life stage of emerging adulthood at ages 18–29 years: implications for mental health. Lancet Psychiatry. 2014;1:569–76.
Hogan DP. The variable order of events in the life course. Am Sociol Rev. 1978;43:573–86.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:587–594.
Zhao L, Ogden CL, Yang Q, Jackson SL, Loria CM, Galuska DA, et al. Association of Usual Sodium Intake with Obesity Among US Children and Adolescents, NHANES 2009-2016. Obesity. 2021;29:587–594.
Eriksen MB, Frandsen TF. The impact of patient, intervention, comparison, outcome (PICO) as a search strategy tool on literature search quality: a systematic review. JMLA. 2018;106:420.
Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions. John Wiley & Sons; 2019.
National Institutes of Health. Study quality assessment tools. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. Accessed 12 Jan 2021.
Faraone SV. Interpreting estimates of treatment effects: implications for managed care. Pharm Therapeutics. 2008;33:700.
Muller K. Statistical power analysis for the behavioral sciences. Taylor & Francis Group; 1989.
Hedberg E. ROBUMETA: stata module to perform robust variance estimation in meta-regression with dependent effect size estimates. 2014. https://EconPapers.repec.org/RePEc:boc:bocode:s457219.
Chen X, Beydoun MA, Wang Y. Is sleep duration associated with childhood obesity? A systematic review and meta-analysis. Obesity. 2008;16:265.
Stoner L, Castro N, Signal L, Skidmore P, Faulkner J, Lark S, et al. Sleep and adiposity in preadolescent children: the importance of social jetlag. Child Obesity. 2018;14:158–164.
Stoner L, Beets MW, Brazendale K, Moore JB, Weaver RG. Social jetlag is associated with adiposity in children. Glob Pediatr Health. 2018;5:2333794X18816921.
Mathew GM, Hale L, Chang A-M. Social jetlag, eating behaviours and BMI among adolescents in the USA. Br J Nutr. 2020;124:979–87.
Urrila AS, Artiges E, Massicotte J, Miranda R, Vulser H, Bézivin-Frere P, et al. Sleep habits, academic performance, and the adolescent brain structure. Sci Rep. 2017;7:1–9.
Chaput J-P, Dutil C. Lack of sleep as a contributor to obesity in adolescents: impacts on eating and activity behaviors. Int J Behav Nutr Phys Act. 2016;13:1–9.
Golley RK, Maher CA, Matricciani L, Olds TS. Sleep duration or bedtime? Exploring the association between sleep timing behaviour, diet and BMI in children and adolescents. Int J Obes (Lond). 2013;37:546–51.
Jarrin DC, McGrath JJ, Drake CL. Beyond sleep duration: distinct sleep dimensions are associated with obesity in children and adolescents. Int J Obes. 2013;37:552.
Arora T, Taheri S. Associations among late chronotype, body mass index and dietary behaviors in young adolescents. Int J Obes. 2015;39:39.
Adamo KB, Wilson S, Belanger K, Chaput J-P. Later bedtime is associated with greater daily energy intake and screen time in obese adolescents independent of sleep duration. J Sleep Disord Ther. 2013;2:2167–0277.1000126.
Keski-Rahkonen A, Kaprio J, Rissanen A, Virkkunen M, Rose RJ. Breakfast skipping and health-compromising behaviors in adolescents and adults. E J Clin Nutr. 2003;57:842.
Hunt ET, Whitfield ML, Brazendale K, Beets MW, Weaver RG. Examining the impact of a summer learning program on children’s weight status and cardiorespiratory fitness: a natural experiment. Eval Program Plann. 2019;74:84–90.
Brazendale K, Beets MW, Turner-McGrievy GM, Kaczynski AT, Pate RR, Weaver RG. Children’s obesogenic behaviors during summer versus school: a within-person comparison. J School Health. 2018;88:886–92.
Tanskey LA, Goldberg JP, Chui K, Must A, Sacheck JM. Accelerated summer weight gain in a low-income, ethnically diverse sample of elementary school children in Massachusetts. Child Obes. 2019;15:244–253.
Mullineaux DR, Wheat J. Research methods: sample size and variability effects on statistical power. Biomechanical Evaluation of Movement in Sport and Exercise: Routledge; 2017. p. 195-220.
Cohn LD, Becker BJ. How meta-analysis increases statistical power. Psychol Methods. 2003;8:243.
Pratt CA, Boyington J, Esposito L, Pemberton VL, Bonds D, Kelley M, et al. Childhood obesity prevention and treatment research (COPTR): interventions addressing multiple influences in childhood and adolescent obesity. Contemp Clin Trials. 2013;36:406–13.
Pratt CA, Loria CM, Arteaga SS, Nicastro HL, Lopez-Class M, de Jesus JM, et al. A systematic review of obesity disparities research. Am J Prev Med. 2017;53:113–122.
Nicholson LM, McLeod Loren D, Reifenberg A, Beets MW, Bohnert AM. School as a protective setting for excess weight gain and child obesity: a meta‐analysis. J Sch Health. 2021;91:19–28.
Evans EW, Bond DS, Pierre DF, Howie WC, Wing RR, Jelalian E. Promoting health and activity in the summer trial: implementation and outcomes of a pilot study. Prev Med Rep. 2018;10:87–92.
Anderson SE, Whitaker RC. Household routines and obesity in US preschool-aged children. Pediatrics. 2010;125:420–8.
Fiese BH, Bost KK. Family ecologies and child risk for obesity: focus on regulatory processes. Fam Rel. 2016;65:94–107.
Jones BL, Fiese BH. Parent routines, child routines, and family demographics associated with obesity in parents and preschool-aged children. Front Psychol. 2014;5:374.
Leech RM, McNaughton SA, Timperio A. Clustering of children’s obesity-related behaviours: associations with sociodemographic indicators. Eur J Clin Nutr. 2014;68:623–8.
Ham SA, Ainsworth BE. Disparities in data on Healthy People 2010 physical activity objectives collected by accelerometry and self-report. Am J Pub Health. 2010;100:S263–S8. S1
Turrisi TB, Bittel KM, West AB, Hojjatinia S, Hojjatinia S, Mama SK, et al. Seasons, weather, and device-measured movement behaviors: a scoping review from 2006 to 2020. Int J Behav Nutr Phys Act. 2021;18:1–26.
Tucker P, Gilliland J. The effect of season and weather on physical activity: a systematic review. Pub Health. 2007;121:909–22.
Rajakumar K, Holick MF, Jeong K, Moore CG, Chen TC, Olabopo F, et al. Impact of season and diet on vitamin D status of African American and Caucasian children. Clin Pediatr (Phila). 2011;50:493–502.
Ma Y, Olendzki BC, Li W, Hafner AR, Chiriboga D, Hebert JR, et al. Seasonal variation in food intake, physical activity, and body weight in a predominantly overweight population. Eur J Clin Nutr. 2006;60:519–28.
Belayneh M, Loha E, Lindtjorn B. Seasonal variation of household food insecurity and household dietary diversity on wasting and stunting among young children in a drought prone area in South Ethiopia: a cohort study. Ecol Food Nutr. 2020;60:1–26.
Erwin D. An analytical study of children’s sleep. Pedagog Semin J Genet Psychol. 1934;45:199–226.
Hjorth MF, Chaput JP, Michaelsen K, Astrup A, Tetens I, Sjödin A. Seasonal variation in objectively measured physical activity, sedentary time, cardio-respiratory fitness and sleep duration among 8-11 year-old Danish children: a repeated-measures study. BMC Pub Health. 2013;13:808.
Ostrin LA, Sajjadi A, Benoit JS. Objectively measured light exposure during school and summer in children. Optom Vis Sci. 2018;95:332–42.
Szymczak J, Jasińska M, Pawlak E, Zwierzykowska M. Annual and weekly changes in the sleep-wake rhythm of school children. Sleep. 1993;16:433–5.
O’Brien KT, Vanderloo LM, Bruijns BA, Truelove S, Tucker P. Physical activity and sedentary time among preschoolers in centre-based childcare: a systematic review. Int J Behav Nutr Phys Act. 2018;15:117.
Hnatiuk JA, Salmon J, Hinkley T, Okely AD, Trost S. A review of preschool children’s physical activity and sedentary time using objective measures. Am J Prev Med. 2014;47:487–97.
Author information
Authors and Affiliations
Contributions
All authors participated in study conception and design. KZ, EH, and CL conducted the searchers and data extraction. RGW completed the data analysis and all authors participated in data interpretation. RGW and KZ complete the manuscript preparation. All authors reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Funding
NIGMS Grant #: 1P20GM130420
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zosel, K., Monroe, C., Hunt, E. et al. Examining adolescents’ obesogenic behaviors on structured days: a systematic review and meta-analysis. Int J Obes 46, 466–475 (2022). https://doi.org/10.1038/s41366-021-01040-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-021-01040-9