Abstract
Background
Children belonging to the same birth cohort (i.e., born in the same year) experience shared exposure to a common obesity-related milieu during the critical early years of development—e.g., secular beliefs and feeding practices, adverse chemical exposures, food access and nutrition assistance policies—that set the stage for a shared trajectory of obesity as they mature. Fundamental cause theory suggests that inequitable distribution of recent efforts to stem the rise in child obesity may exacerbate cohort-based disparities over time.
Methods
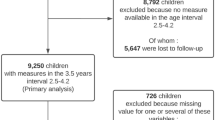
Data were from electronic health records spanning 2007–2016 linked to birth records for children ages 2–19 years. We used hierarchical age-period-cohort models to investigate cohort effects on disparities in obesity related to maternal education. We hypothesized that maternal education-based disparities in prevalence of obesity would be larger among more recent birth cohorts.
Results
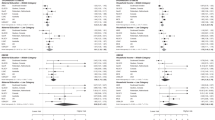
Sex-stratified models adjusted for race/ethnicity showed substantial obesity disparities by maternal education that were evident even at young ages: prevalence among children with maternal education < high school compared to maternal college degree was approximately three times as high among girls and twice as high among boys. For maternal education < high school, disparities compared to maternal college degree were higher in more recent birth cohorts. Among girls, this disparity cohort effect was evident at younger ages (at age 4, the disparity increased by 4 [0.1–8] percentage points per 5 birth years), while among boys it was larger at older ages (at age 16, the disparity increased by 7 [1–14] percentage points per 5 birth years).
Conclusions
There may be widening maternal education-based disparities in child obesity by birth cohort at some ages.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity among adults and youth: United States, 2015-2016. NCHS Data Brief. 2017;288:1–8.
Must A, Strauss RS. Risks and consequences of childhood and adolescent obesity. Int J Obes Relat Metab Disord. 1999;23:S2–11.
Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB. Years of life lost due to obesity. JAMA. 2003;289:187–93.
Freedman DS, Khan LK, Dietz WH, Srinivasan SR, Berenson GS. Relationship of childhood obesity to coronary heart disease risk factors in adulthood: the Bogalusa Heart Study. Pediatrics. 2001;108:712–8.
Ogden CL, Carroll MD, Fakhouri TH, Hales CM, Fryar CD, Li X, et al. Prevalence of obesity among youths by household income and education level of head of household—United States 2011-2014. Morb Mortal Wkly Rep. 2018;67:186–9.
Foster BA, Maness TM, Aquino CA. Trends and disparities in the prevalence of childhood obesity in South Texas between 2009 and 2015. J Obes. 2017;2017:1424968.
Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL. Trends in obesity and severe obesity prevalence in us youth and adults by sex and age, 2007-2008 to 2015-2016. JAMA. 2018;319:1723–5.
Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran D, Kit BK, et al. Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. JAMA. 2016;315:2292–9.
Robbins JM, Mallya G, Wagner A, Buehler JW. Prevalence, disparities, and trends in obesity and severe obesity among students in the school district of Philadelphia, Pennsylvania, 2006-2013. Prev Chronic Dis. 2015;12:E134.
Skinner AC, Perrin EM, Skelton JA. Prevalence of obesity and severe obesity in US children, 1999-2014. Obesity. 2016;24:1116–23.
Weedn AE, Hale JJ, Thompson DM, Darden PM. Trends in obesity prevalence and disparities among low-income children in Oklahoma, 2005–2010. Child Obes. 2014;10:318–25.
Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995;80–94. Extra Issue.
Halfon N, Hochstein M. Life course health development: an integrated framework for developing health, policy, and research. Milbank Q. 2002;80:433–79.
Halfon N, Forrest CB, Lerner RM, Faustman EM (ed.). Handbook of life course health development. Cham: Springer; 2018.
Keyes KM, Utz RL, Robinson W, Li G. What is a cohort effect? Comparison of three statistical methods for modeling cohort effects in obesity prevalence in the United States, 1971–2006. Soc Sci Med. 2010;70:1100–8.
Barker DJ. The fetal and infant origins of adult disease. BMJ. 1990;301:1111.
Keith SW, Redden DT, Katzmarzyk PT, Boggiano MM, Hanlon EC, Benca RM, et al. Putative contributors to the secular increase in obesity: exploring the roads less traveled. Int J Obes. 2006;30:1585–94.
Yang Y, Land KC. In: Keiding N, Morgan BJT, Wikle CK, van der Heijden P, editors. Age-period-cohort analysis: new models, methods, and empirical applications. Boca Raton: CRC Press; 2013.
Adler NE, Newman K. Socioeconomic disparities in health: pathways and policies. Health Aff. 2002;21:60–76.
Cochrane SH, Leslie J, O’Hara DJ. Parental education and child health: intracountry evidence. Health Policy Educ. 1982;2:213–50.
Silvestrin S, Silva CH, Hirakata VN, Goldani AA, Silveira PP, Goldani MZ. Maternal education level and low birth weight: a meta-analysis. J Pediatr. 2013;89:339–45.
Roos LL, Walld R, Wajda A, Bond R, Hartford K. Record linkage strategies, outpatient procedures, and administrative data. Med Care. 1996;34:570–82.
Centers for Disease Control and Prevention. Childhood obesity facts: Centers for Disease Control and Prevention. 2018. https://www.cdc.gov/obesity/data/childhood.html.
Centers for Disease Control and Prevention. A SAS Program for the 2000 CDC growth charts (ages 0 to <20 years). 2019. https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm.
Daymont C, Ross ME, Russell Localio A, Fiks AG, Wasserman RC, Grundmeier RW. Automated identification of implausible values in growth data from pediatric electronic health records. J Am Med Inform Assoc. 2017;24:1080–7.
Cheung MW, Jak S. Analyzing big data in psychology: a split/analyze/meta-analyze approach. Front Psychol. 2016;7:738.
Harper S, Lynch J, Meersman SC, Breen N, Davis WW, Reichman ME. An overview of methods for monitoring social disparities in cancer with an example using trends in lung cancer incidence by area-socioeconomic position and race-ethnicity, 1992–2004. Am J Epidemiol. 2008;167:889–99.
Messer LC. Invited commentary: measuring social disparities in health-what was the question again? Am J Epidemiol. 2008;167:900–4.
Keppel K, Pamuk E, Lynch J, Carter-Pokras O, Kim I, Mays V, et al. Methodological issues in measuring health disparities. Vital Health Stat. 2005;2:1–16.
US Census Bureau. American Community Survey, S1501: Educational Attainment. 2015. https://data.census.gov/cedsci/.
US Census Bureau. American Community Survey, S2704: Public Health Insurance Coverage by Type. 2015. https://data.census.gov/cedsci/.
Kharofa RY, Klein JA, Khoury P, Siegel RM. Severe obesity decreasing in children in Cincinnati, Ohio. Clin Pediatr. 2017;56:752–8.
Bailey LC, Milov DE, Kelleher K, Kahn MG, Del Beccaro M, Yu F, et al. Multi-institutional sharing of electronic health record data to assess childhood obesity. PLoS ONE. 2013;8:e66192.
Lemas DJ, Cardel MI, Filipp SL, Hall J, Essner RZ, Smith SR, et al. Objectively measured pediatric obesity prevalence using the OneFlorida Clinical Research Consortium. Obes Res Clin Pract. 2019;13:12–5.
Koebnick C, Mohan YD, Li X, Young DR. Secular trends of overweight and obesity in young Southern Californians 2008-2013. J Pediatr. 2015;167:1264–71.e2.
Wen X, Gillman MW, Rifas-Shiman SL, Sherry B, Kleinman K, Taveras EM. Decreasing prevalence of obesity among young children in Massachusetts from 2004 to 2008. Pediatrics. 2012;129:823–31.
Robert Wood Johnson Foundation. Obesity rates for youth ages 10 to 17: Robert Wood Johnson Foundation. 2019. https://stateofchildhoodobesity.org/children1017/.
Edmunds LS, Woelfel ML, Dennison BA, Stratton H, Pruzek RM, Abusabha R. Overweight trends among children enrolled in the New York State special supplemental nutrition program for women, infants, and children. J Am Diet Assoc. 2006;106:113–7.
Centers for Disease Control and Prevention. Vital signs: obesity among low-income, preschool-aged children—United States, 2008-2011. Morb Mortal Wkly Rep. 2013;62:629–34.
Mei Z, Scanlon KS, Grummer-Strawn LM, Freedman DS, Yip R, Trowbridge FL. Increasing prevalence of overweight among US low-income preschool children: the Centers for Disease Control and Prevention pediatric nutrition surveillance, 1983 to 1995. Pediatrics. 1998;101:E12.
Sherry B, Mei Z, Scanlon KS, Mokdad AH, Grummer-Strawn LM. Trends in state-specific prevalence of overweight and underweight in 2- through 4-year-old children from low-income families from 1989 through 2000. Arch Pediatr Adolesc Med. 2004;158:1116–24.
Ogden CL, Lamb MM, Carroll MD, Flegal KM. Obesity and socioeconomic status in children and adolescents: United States, 2005-2008. NCHS Data Brief. 2010;51:1–8.
Wang Y. Disparities in pediatric obesity in the United States. Adv Nutr. 2011;2:23–31.
An R, Xiang X. Age-period-cohort analyses of obesity prevalence in US adults. Public Health. 2016;141:163–9.
Heo J, Beck AN, Lin SF, Marcelli E, Lindsay S, Karl Finch B. Cohort-based income gradients in obesity among U.S. adults. Am J Hum Biol. 2018;30. https://doi.org/10.1002/ajhb.23084. Epub 2017 Nov 27.
Reither EN, Hauser RM, Yang Y. Do birth cohorts matter? Age-period-cohort analyses of the obesity epidemic in the United States. Soc Sci Med. 2009;69:1439–48.
Kwok MK, Tu YK, Kawachi I, Schooling CM. Age-period-cohort analysis of trends in blood pressure and body mass index in children and adolescents in Hong Kong. J Epidemiol Community Health. 2017;71:1161–8.
Hosseini M, Kelishadi R, Baikpour M, Ataei N, Qorbani M, Yousefifard M, et al. Age-period-cohort analysis of obesity and overweight in Iranian children and adolescents. Int J Endocrinol Metab. 2017;15:e13561.
Bell A, Jones K. Don’t birth cohorts matter? A commentary and simulation exercise on Reither, Hauser, and Yang’s (2009) age-period-cohort study of obesity. Soc Sci Med. 2014;101:176–80.
Bell A, Jones K. Age, period and cohort processes in longitudinal and life course analysis: a multilevel perspective. In: Burton-Jeangros C, Cullati S, Sacker A, Blane D, editors. A life course perspective on health trajectories and transitions. Cham: Springer, 2015. pp. 197–213.
IOM (Institute of Medicine). Capturing social and behavioral domains and measures in electronic health records: Phase 2. Washington, DC: The National Academies Press; 2014.
Data Resource Center for Child & Adolescent Health. NSCH Interactive Data Query (2016 - Present) Baltimore, MD: Data Resource Center for Child & Adolescent Health; 2020 [cited 2020 December 3]. Available from: https://www.childhealthdata.org/browse/survey.
Josberger RE, Wu M, Nichols EL. Birth certificate validity and the impact on primary cesarean section quality measure in New York State. J Community Health. 2019;44:222–9.
Northam S, Knapp TR. The reliability and validity of birth certificates. J Obstet Gynecol Neonatal Nurs. 2006;35:3–12.
Ogden CL, Fryar CD, Hales CM, Carroll MD, Aoki Y, Freedman DS. Differences in obesity prevalence by demographics and urbanization in US children and adolescents, 2013-2016. JAMA. 2018;319:2410–8.
Acknowledgements
This study is part of the Pediatric Big Health Data initiative funded by the State of Pennsylvania and led by the Children’s Hospital of Philadelphia, University of Pennsylvania, and the Urban Health Collaborative at Drexel University. We would like to thank the investigators of the Pediatric Big Health Data initiative for their contributions. These individuals include: Christopher B. Forrest, MD, Ph.D.; L. Charles Bailey, MD, Ph.D.; Shweta P. Chavan, MSEE; Rahul A. Darwar, MPH; Jillian Benedetti, MPH; Daniel Forsyth; Chén C. Kenyon, MD, MSHP; Ritu Khare, Ph.D.; Mitchell G. Maltenfort, Ph.D.; Aaron J. Masino, Ph.D., ME; Xueqin Pang, Ph.D.; Ting Qian, Ph.D.; Hanieh Razzaghi, MPH; Justine Shults, Ph.D.; Levon H. Utidjian, MD, MBI from the Children’s Hospital of Philadelphia; Ana V. Diez Roux, MD, Ph.D., MPH; Amy H. Auchincloss, Ph.D., MPH; Elizabeth A. Campbell, MSPH; Kimberly Daniels, MS; Anneclaire J. De Roos, Ph.D., MPH; J. Felipe Garcia-Espana, MS, Ph.D.; Irene Headen, Ph.D., MS; Félice Lê-Scherban, Ph.D., MPH; Steven Melly, MS, MA; Yvonne L. Michael, ScD, SM; Jeffrey Moore, MS; Kari Moore, MS; Abigail E. Mudd, MPH; Leah Schinasi, Ph.D., MSPH; and Yuzhe Zhao, MS from Drexel University and, Yong Chen, Ph.D.; John H. Holmes, Ph.D.; Rebecca A. Hubbard, Ph.D.; A. Russell Localio, JD, MPH, Ph.D. from the University of Pennsylvania. This work was supported by a grant from the Commonwealth Universal Research Enhancement (CURE) program funded by the Pennsylvania Department of Health—2015 Formula award—SAP #4100072543.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Lê-Scherban, F., Moore, J., Headen, I. et al. Are there birth cohort effects in disparities in child obesity by maternal education?. Int J Obes 45, 599–608 (2021). https://doi.org/10.1038/s41366-020-00724-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-020-00724-y
This article is cited by
-
Risk factors of persistent adolescent thinness: findings from the UK Millennium Cohort Study
BMC Public Health (2023)
-
Clustering Based BMI Indexing for Child Disease Prone-Probability Prediction
SN Computer Science (2023)