Abstract
Introduction
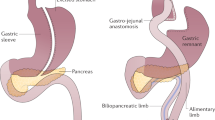
Bariatric surgery (BS) produces superior weight loss compared to non-surgical interventions. However, studies suggest bariatric patients who have undergone gastric-bypass surgery have an increased risk of developing new onset substance use disorder (SUD) or suffer negative outcomes after surgery. As such, many bariatric programs consider alcohol/ illicit drug misuse a contraindication to BS. The purpose of this systematic review was to investigate weight loss outcomes, post-surgery substance use patterns and other morbidity/mortality in BS patients with a history of substance use/SUD.
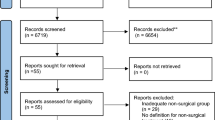
Methods
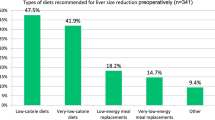
Studies were identified by searching Ovid Medline(R), Embase, and PsychInfo. We included all study types investigating humans of any age/sex who had undergone any BS procedure with data regarding substance use before and/or after surgery. Outcome measures included metabolic outcomes and psychiatric outcomes after bariatric surgery in patients reporting substance use prior to bariatric surgery and substance use patterns after bariatric surgery.
Results
Fifty-eight studies were included in the review. Studies reporting weight loss after BS did not demonstrate an association between substance use and negative weight loss outcomes. Several studies reported a significant portion of participants having new onset or increased substance use after BS. Factors associated with new onset or increased substance use/SUD after BS included the type of surgery, a history of SUD, a family history of SUD, coping skills/life stressors, age, male sex and alcohol sensitization after surgery.
Conclusion
Substance use history does not appear to influence weight loss after BS, however it may contribute to increased substance use after BS. Clinicians should ensure valid screening tools when assessing BS candidates for substance use history and ensure long term follow-up care post-operatively.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Sheets CS, Peat CM, Berg KC, White EK, Bocchieri-Ricciardi L, Chen EY, et al. Post- operative psychosocial predictors of outcome in bariatric surgery. Obes Surg. 2015;25:330–45.
Dawes AJ, Maggard-Gibbons M, Maher AR, Booth MJ, Miake-Lye I, Beroes JM, et al. Mental health conditions among patients seeking and underoing bariatric surgery. JAMA. 2016;315:150–63.
Parikh M, Johnson JM, Ballem N. ASMBS position statement on alcohol use before and after bariatric surgery. Surg Obes Relat Dis. 2016;12:225–30.
Taylor VH. Weighty matters: the association between mental health, pregnancy, and obesity. J Popul Ther Clin Pharmacol. 2012;19:e483–7.
Oprah.com, “Suddenly Skinny”. 10/24/2006, http://www.oprah.com/oprahshow/suddenly-skinny/all%20accessed%20December%2013.Accessed Dec 2017.
Spadola CE, Wagner EF, Dilon FR, Trepka MJ, Cruz-Munoz N, Messiah SE. Alcohol and drug use among postoperative bariatric patients: a systematic review of the emerging research and its implications. Alcohol Clin Exp Res. 2015;39:1582–601.
Heinberg LJ, Ashton K, Coughlin J. Alcohol and bariatric surgery: review and suggested recommendations for assessment and management. Surg Obes Relat Dis. 2012;8:357–63.
Steffen KJ, Engel SG, Wonderlich JA, Pllert GA, Sondag C. Alcohol and other addictive disorders following bariatric surgery, risk factors and possible etiologies. Eur Eat Disord Rev. 2015;23:442–50.
Li L, Wi L. Substance use after bariatric surgery: A review. J Psychiatr Res. 2016;76:16–29.
Ali M, El Chaar M, Ghiassi S, Rogers AM. American society for metabolic and bariatric surgery updated position statement on sleeve gastrectomy as a bariatric procedure. Surg Obes Relat Dis. 2017;13:1652–57.
Thomas BH, Ciliska D, Dobbins M, Micucci S. A process for systematically reviewing the literature: providing the research evidence for public health nursing interventions. Worldviews Evid Based Nurs. 2004;1:176–84.
Burgos MG, Cabral PC, Maio R, Oliveira BM, Dias MS, Melim DB, et al. Prevalence of alcohol abuse before and after bariatric surgery associated with nutritional and lifestyle factors: a study involving a portuguese population. Obes Surg. 2015;25:1716–22.
Mitchell JE, Steffen K, Engel S, King WC, Chen JY, Winters K, et al. Addictive disorders after Roux-En-Y gastric bypass. Surg Obes Relat Dis. 2015;11:897–905.
Tedesco M, Hua WQ, Lohnberg JA, Bellatorre N. A Prior History of Substance Abuse in Veterans Undergoing Bariatric Surgery.” J Obes. 2013; 740312.
Lent MR, Hayes SM, Wood GC, Napolitano MA, Argyropoulos G, Gerhard GS, et al. Smoking and alcohol use in gastric bypass patients. Eat Behav. 2013;14:460–3.
Sanchez-Cabezudo Diaz-Guerra C, Larrad Jimenez A. Analysis of weight loss with the biliopancreatic diversion of larrad: absolute failures or relative successes? Obes Surg. 2002;12:249–52.
Yanos BR, Saules KK, Schuh LM. Predictors of lowest weight and long-term weight regain among roux-en-y gastric bypass patients. Obes Surg. 2015;25:1364–70.
Odom J, Zalesin KC, Washington TL, Miller WW, Hakmeh B, Zaremba DL, et al. Behavioral predictors of weight regain after bariatric surgery. Obes Surg. 2010;20:349–56.
Vidot DC, Prado G, De La Cruz-Munoz N, Spadola C, Cuesta M. Postoperative marijuana use and disordered eating among bariatric surgery patients. Surg Obes Relat Dis. 2016;12:171–8.
Adams CE, Gabriele JM, Baillie LE. Tobacco use and substance use disorders as predictors of postoperative weight loss 2 years after bariatric surgery. J Behav Health Serv Res. 2012;39:462–71.
Kalarchian MA, Marcus MD, Levine MD, Soulakova JN, Courcoulas AP. Relationship of psychiatric disorders to 6-Month outcomes after gastric bypass. Surg Obes Relat Dis. 2008;4:544–9.
Marek RJ, Tarescavage AM, Ben-Porath YS, Ashton K, Merrell RJ, Heinberg LJ. Using presurgical psychological testing to predict 1-Year appointment adherence and weight loss in bariatric surgery patients: predictive validity and methodological considerations. Surg Obesity Relat Dis. 2015;11:1171–81.
Hayden MJ, Murphy KD, Brown WA. Axis I disorders in adjustable gastric band patients: the relationship between psychopathology and weight Loss. Obes Sug. 2014;24:1469–75.
Kalarchian MA, King WC, Devlin MJ, Marcus MD, Garcia L, Chen JY, et al. Psychiatic disorders and weight change in a prospective study of bariatric surgery patients: a 3-year follow-up. Psychosom. Med. 2016;78:373–81.
Pulcini ME, Saules KK. Roux-en-y gastric bypass patients hospitalized for substance use disorders achieve successful weight loss despite poor psychosocial outcomes. Clin Obes. 2013;3:95–102.
Marek RJ, Ben-Porath YS, van Dulmen M, Ashton K, Heinberg HJ. Using the presurgical psychological evaluation to predict 5-year weight loss outcomes in bariatric surgery patients. Surg Obes Relat Dis. 2017;13:514–21.
Reslan S, Saules KK, Greenwald MK. Substance misuse following roux-en-y gastric bypass surgery. Subst Use Misuse. 2014;49:405–17.
Heinberg LJ, Ashton K. History of substance abuse relates to improved postbariatric body mass index outcomes. Surg Obes Relat Dis. 2010;6:417–21.
Clark MM, Balsiger BM, Sletten CD, Dahlman KL, Ames G, Williams DE, et al. Psychosocial factors and 2-year outcome following bariatric surgery for weight loss. Obes Surg. 2003;13:739–45.
Conason A, Teixeira J, Hsu CH, Puma L, Knafo D. Substance use following bariatric weight loss surgery. JAMA Surg. 2013;148:145–50.
King WC, Chen JY, Mitchell JE, Kalarchian MA, Steffen KJ, Engel SG, et al. Prevalence of alcohol use disorders before and after bariatric surgery. JAMA. 2012;307:2516–25.
King WC, Chen JY, Courcoulas AP, Dakin GF, Engel SG, Flum DR, et al. Alcohol and other substance use after bariatric surgery: prospective evidence from a US multicenter cohort study. Surg Obes Relat Dis. 2017;13:1392–404.
Kovacs Z, Valentin JB, Nielsen RE. Risk of psychiatric disorders, self-harm behavior and service use associated with bariatric surgery. Acta Psychiatre Scand. 2017;135:149–58.
Suzuki J, Haimovici F, Chang G. Alcohol use disorders after bariatric surgery. Obes Surg. 2012;22:201–7.
Smith KE, Engel SG, Steffen KJ, Garcia L, Grothe K, Koball A, et al. Problematic alcohol use and associated characteristic following bariatric surgery. Obes Surg. 2018;28:1248–54.
Wiedemann AA, Saules KK, Ivezaj V. Emergence of new onset substance use disorders among post-weight loss surgery patients. Clin Obes. 2013;3:194–201.
Cuellar-Barboza AB, Frye MA, Grothe K, Prieto ML, Schneekloth TD, Loukianova LL, et al. Change in consumption patterns for treatment-seeking patients with alcohol use disorder post-bariatric surgery. J Psychosom Res. 2015;78:199–204.
Saules KK, Wiedemann A, Ivezaj V, Hopper JA, Foster-Hartsfield J. Bariatric surgery history among substance abuse treatment patients: prevalence and associated features. Surg Obes Relat Dis. 2010;6:615–21.
Backman O, Stockeld D, Rasmussen F, Naslund E, Marsk R. Alcohol and substance abuse, depression and suicide attempts after roux-en-y gastric bypass surgery. BJS. 2016;103:1336–42.
Gribsholt SB, Svensson E, Richelsen B, Raundahl U, Sorensen HT, Thomsen RW. Rate of acute hospital admissions before and after roux-en-y gastric bypass surgery. Ann. Surg. 2018;267:319–25.
Spadola CE, Wagner EF, Accornero VH, Vidot DC, Cruz-Munoz NF, Messiah SE. Alcohol use patterns and alcohol use disorders among young adult, ethnically diverse bariatric surgery patients. Subst Abus. 2017;38:82–87.
Ivezaj V, Saules KK. New-onset substance use disorder after gastric bypass surgery: rates and associated characteristics. Obe Surg. 2014;24:1975–80.
Bhatti JA, Nathens AB, Thiruchelvan D, Redelmeier DA. Weight loss surgery and subsequent emergency care use: a population-based cohort study. Am J. Emerg Med. 2016;34:861–5.
Zeller MH, Washington GA, Mitchell JE, Sarwer DB, Reiter-Purtill J, Jenkins TM, et al. Alcohol use risk in adolescents 2 years after bariatric surgery. Surg Obes Relat Dis. 2017;13:85–94.
Wendling A, Wudyka A. Narcotic addiction following gastric bypass surgery-a case study. Obes Surg. 2011;21:680–3.
Higa KD, Ho T, Boone KB, Roubicek MC. Narcotic withdrawal syndrome following gastric bypass - a difficult diagnosis. Obes Surg. 2001;11:631–4.
Fogger SA, McGuinness TM. The Relationship between addictions and bariatric surgery for nurses in recovery. Perspect Psychiatr Care. 2012;48:10–5.
Ostlund MP, Backman O, Marsk R, Stockeld D, Lagergren J, Rasmussen F, et al. Increased admission for alcohol dependence after gastric bypass surgery compared with restrictive bariatric surgery. JAMA Surg. 2013;148:374–7.
Svensson PA, Anveden A, Romeo S, Peltonen M, Ahlin S, Burza MA, et al. Alcohol consumption and alcohol problems after bariatric surgery in the swedish obese subjects study. Obesity. 2013;21:2444–51.
Raebel MA, Newcomer SR, Bayliss EA, Boudreau D, DeBar L, Elliott TE, et al. Chronic opioid use emerging after bariatric surgery. Pharmacoepidemiol Drug Saf. 2014;23:1247–57.
Spadola CE, Wagner EF, Varga LM, Syvertsen JL, Cruz-Munoz NF, Messiah SE. A qualitative examination of increased alcohol use after bariatric surgery among racially/ethnically diverse young adults. Obes Surg. 2018;12:1492–7.
Yoder R, MacNeela P, Conway R, Heary C. How do individuals develop alcohol use disorder after bariatric surgery? A grounded theory explanation. Obes Surg. 2018;28:717–24.
Zeller MH, Pendery EC, Reiter-Purtill J, Hunsaker SL, Jenkins TM, Helmrath MA, et al. From adolescence to young adulthoot: trajectories of psychosocial health following roux-en-y gastric bypass. Surg Obes Relat Dis. 2017;13:1196–203.
Fowler L, Ivezaj V, Saules KK. Problematic intake of high-sugar/low-fat and high glycemic index foods by bariatric patients is associated with development of post-surgical new onset substance use disorders. Eat Behav. 2014;15:505–8.
Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The alcohol use disorders identification test, guidelines for use in primary care. World Health Organization, Department of Mental Health and Substance Dependence. 2001 2nd edition, 10–11.
Westermeyer J, Yargic I, Thuras P. Michigan assessment-screening test for alcohol and drugs (MAST/AD): evaluation in a clinical sample. Am J Addict. 2012;12:151–62.
WHO ASSIST Working Group. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): development, reliability and feasibility. Addiction. 2002;97:1183–94.
Watkins BJ, Blackmun S. Gastric adenocarcinoma after roux-en-y gastric bypass: access and evaluation of excluded stomach. Surg Obes Relat Dis. 2007;3:644–7.
Still CD, Wood GC, Chu X, Manney C, Strodel W, Petrick A, et al. Clinical factors associated with weight loss outcomes after roux-en-y gastric bypass surgery. Obesity. 2014;22:888–94.
Talem DA, Talamini M, Gesten F, Patterson W, Peoples B, Gracia G, et al. Hospital admissions greater than 30 days following bariatric surgery: patient and procedure matter. Surg Endosc. 2015;29:1310–5.
Diniz Mde F, Moura LD, Kelles SM, Diniz MT. Long-term mortality of patients submitted to roux-en-y gastric bypass in public health system: high prevalence of alcoholic cirrhosis and suicides. Arq Bras de Cir Dig. 2013;26(Suppl 1):53–6.
Totte E, Hendrickx L, Van Hee R. Biliopancreatic diversion for treatment of morbid obesity: experience in 180 consecutive cases. Obes Surg. 1999;9:161–5.
Ortega J, Fernandez-Canet R, Alvarez-Valdeita S, Cassinello N. Predictors of psychological symptoms in morbidly obese patients after gastric bypass surgery. Surg Obes Relat Dis. 2012;8:770–6.
Nandipati K, Lin E, Husain F, Perez S, Srinivasan J, Sweeney JF. Factors predicting the increased risk for return to the operating room in bariatric patients: A NSQIP database study. Surg Endos. 2013;27:1172–7.
Nakamura KM, Haglind EG, Clowes JA, Achenbach SJ, Atkinson EJ, Melton LJ. Fracture risk following bariatric surgery: A population-based study. Osteoporos Int. 2014;25:151–8.
Benotti P, Wood GC, Winegar DA, Petrick AT, Still CD, Argyropoulos G, et al. Risk factors associated with mortality after roux-en-y gastric bypass surgery. Ann Surg. 2014;259:123–30.
Brolin RE, Asad M. Rationale for reversal of failed bariatric operations. Surg Obes Relat Dis. 2009;5:673–6.
Segal A, Hilton Libanori HT, Azevedo A. Bariatric surgery in a patient with possible psychiatric contraindications. Obes Surg. 2002;12:598–601.
Ivezaj V, Saules KK, Wiedemann AA. I didn’t see this coming: why are postbariatric patients in substance abuse treatment? Patients’ perceptions of etiology and future recommendations. Obes Surg. 2012;22:1308–14.
Dutta S, Morton J, Shepard E, Peebles R, Farrales-Nguyen S, Hammer LD. Methamphetamine use following bariatric surgery in an adolescent. Obes Surg. 2006;16:780–2.
Ramanan B, Gupta PK, Gupta H, Fang X. Development and validation of a bariatric surgery mortality risk calculator. J Am Coll Surg. 2012;214:892–900.
Signorini FJ, Polero V, Viscido G, Navarro L, Obeide L, Moser F. Long-term relationship between tobacco use and weight loss after sleeve gastrectomy. Obes Surg. 2018;28:2644–49.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Kanji, S., Wong, E., Akioyamen, L. et al. Exploring pre-surgery and post-surgery substance use disorder and alcohol use disorder in bariatric surgery: a qualitative scoping review. Int J Obes 43, 1659–1674 (2019). https://doi.org/10.1038/s41366-019-0397-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-019-0397-x
This article is cited by
-
Pre-Operative Substance Use Disorder is Associated with Higher Risk of Long-Term Mortality Following Bariatric Surgery
Obesity Surgery (2023)
-
Substance abuse screening prior to bariatric surgery: an MBSAQIP cohort study evaluating frequency and factors associated with screening
Surgical Endoscopy (2023)
-
Incidence of Substance Use Disorder Following Bariatric Surgery: A Retrospective Cohort Study
Obesity Surgery (2023)
-
Guidelines for Perioperative Care in Bariatric Surgery: Enhanced Recovery After Surgery (ERAS) Society Recommendations: A 2021 Update
World Journal of Surgery (2022)
-
Substance Use, Mental Health, and Weight-Related Behaviors During the COVID-19 Pandemic Among Metabolic and Bariatric Surgery Patients
Obesity Surgery (2021)