Abstract
Prehypertension—blood pressure between 120–139/80–89 mmHg—is a major public health concern. The condition is very prevalent (especially in obese young people), is often associated with other cardiovascular risk factors and independently increases the risk of hypertension and subsequent cardiovascular events. In the general population, prehypertension can be lowered, but not often reliably, by lifestyle modifications. Drug therapy for prehypertension is not yet recommended, except for individuals with diabetes, chronic kidney disease, and perhaps known coronary artery disease, because of short-term cost considerations and unproven long-term benefits. Ongoing research will probably identify which individuals with blood pressures in the prehypertensive range, but with no serious comorbidities, would benefit from treatment. In this Review, we attempt to summarize the recently published data concerning the epidemiology, attendant risks and potential treatment options for this important and growing public-health problem.
Key Points
-
Prehypertension is the term used by the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure to define persistent office blood pressures between 120–139/80–89 mmHg, inclusive
-
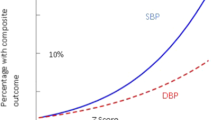
In comparison with people who have normal blood pressures (<120/80 mmHg), individuals with blood pressure in the prehypertensive range are more likely to have other cardiovascular risk factors, develop sustained hypertension, require pharmacological therapy to reduce their blood pressure, and have raised cardiovascular event risk
-
Lifestyle modifications, including weight loss, sodium restriction and other dietary measures should be recommended to, and adopted by, all individuals with prehypertension or hypertension
-
Although the feasibility of drug therapy for prehypertension has been shown, the risk:benefit ratio is uncertain, and the cost would be high
-
Future studies (including PILL and AVIATOR studies) might help clarify the potential role of drug therapy for prehypertension
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Chobanian AV et al. (2003) The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 Report. JAMA 289: 2560–2572
Chobanian AV et al. (2003) Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. National High Blood Pressure Education Program Coordinating Committee. Hypertension 42: 1206–1252
Whitworth JA ; for the World Health Organization, International Society of Hypertension Writing Group (2003) 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens 21: 1983–1992
The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) (2007) 2007 Guidelines for the management of arterial hypertension. Eur Heart J 28: 1462–1536
Williams B et al. (2004) British Hypertension Society guidelines for hypertension management 2004 (BHS-IV): summary. BMJ 328: 634–640
Saruta T (2005) The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2004) [Japanese]. Nippon Rinsho 63: 952–958
Hemmelgarn BR et al. (2006) The 2006 Canadian Hypertension Education Program recommendations for the management of hypertension: part 1—blood pressure measurement, diagnosis and assessment of risk. Can J Cardiol 22: 573–581
Giles T et al. (2005) Expanding the definition and classification of hypertension. J Clin Hypertens (Greenwich) 7: 505–512
Lewington S et al.; Prospective Studies Collaboration (2002) Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 360: 1903–1913
Fields LE et al. (2004) The burden of adult hypertension in the United States 1999 to 2000: a rising tide. Hypertension 44: 398–404
Vasan RS et al. (2002) Residual lifetime risk for developing hypertension in middle-aged women and men: The Framingham Heart Study. JAMA 287: 1003–1010
Svetkey LP (2005) Hypertension grand rounds: management of prehypertension. Hypertension 45: 1056–1061
Atilla K and Vasan RS (2006) Prehypertension and risk of cardiovascular disease. Expert Rev Cardiovasc Ther 4: 111–117
Qureshi AI et al. (2005) Prevalence and trends of prehypertension and hypertension in United States: National Health and Nutrition Examination Surveys 1976 to 2000. Med Sci Monitor 11: CR403–CR409
Hajjar I and Kotchen TA (2003) Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988-2000. JAMA 290: 199–203
Zhang Y et al. (2006) Prehypertension, diabetes and cardiovascular disease risk in a population-based sample: The Strong Heart Study. Hypertension 47: 410–414
Grotto I et al. (2006) Prevalence of prehypertension and associated cardiovascular risk profiles among young Israeli adults. Hypertension 48: 254–259
Tsai P-S et al. (2005) Prevalence and determinants of prehypertensive status in the Taiwanese general population. J Hypertens 23: 1355–1360
Wang Y and Wang QJ (2004) The prevalence of prehypertension and hypertension among US adults according to the new Joint National Committee guidelines. Arch Intern Med 164: 2126–2134
Greenlund KJ et al. (2004) Prevalence of heart disease and stroke risk factors in persons with prehypertension in the United States, 1999-2000. Arch Intern Med 164: 2113–2118
Lee JY et al. (2006) Comparison of risk factors between prehypertension and hypertension in Korean male industrial workers. Public Health Nurs 23: 314–323
Okosun IS et al. (2004) Racial/ethnic differences in prehypertension in American adults: population and relative attributable risks of abdominal obesity. J Hum Hypertens 18: 849–855
Israeli E et al. (2006) Prehypertension and obesity in adolescents: a population study. Am J Hypertens 19: 708–712
Choi KM et al. (2006) Prevalence of prehypertension and hypertension in a Korean population: Korean National Health and Nutrition Survey 2001. J Hypertens 24: 1515–1521
Chockalingam A et al. (2005) Patterns and predictors of prehypertension among “healthy'' urban adults in India. Angiology 56: 557–563
Ramos E and Barros H (2005) Prevalence of hypertension in 13-year-old adolescents in Porto, Portugal. Revis Port Cardiol 24: 1075–1087
Seo H-J et al. (2006) The incidence and risk factors of hypertension that developed in a male-workers' cohort for 3 years [Korean]. J Prev Med Pub Health/Yebang Uihakhoe Chi 39: 229–234
Kanauchi M et al. (2004) Metabolic syndrome and new category 'pre-hypertension' in a Japanese population. Curr Med Res Opin 20: 1365–1370
Cordero A et al. (2006) Prehypertension is associated with insulin resistance state and not with an initial renal function impairment: a Metabolic Syndrome in Active Subjects in Spain (MESYAS) Registry substudy. Am J Hypertens 19: 189–196
Jago R et al. (2006) Prevalence of abnormal lipid and blood pressure values among an ethnically diverse population of eighth-grade adolescents and screening implications. Pediatrics 117: 2065–2073
Chrysohoou C et al. (2004) Association between prehypertension status and inflammatory markers related to atherosclerotic disease: The ATTICA Study. Am J Hypertens 17: 568–573
King DE et al. (2004) Elevation of C-reactive protein in people with prehypertension. J Clin Hypertens (Greenwich) 6: 562–568
Papadopoulos DP et al. (2005) Adiponectin and resistin plasma levels in healthy individuals with prehypertension. J Clin Hypertens (Greenwich) 7: 729–733
Toikka JO et al. (2000) Increased arterial intima-media thickness and in vivo LDL oxidation in young men with borderline hypertension. Hypertension 36: 929–933
Cornelissen G et al. (2005) Opportunity of detecting pre-hypertension: worldwide data on blood pressure overswinging. Biomed Pharmacother 59 (Suppl 1): S152–S157
Otsuka K et al. (2003) Clinical chronobiology and chronome-geriatrics at variance with recommendations of subsequent guidelines, yet focusing indeed on pre-hypertension in the physiological range. Biomed Pharmacother 57 (Suppl 1): S164–S198
Cugini P et al. (1998–1999) 'Minimal-change hypertensive retinopathy' and 'arterial pre-hypertension', illustrated via ambulatory blood-pressure monitoring in putatively normotensive subjects. Internat Ophthalmol 22: 145–149
Ikram MK et al. (2006) Retinal vessel diameters and risk of hypertension: The Rotterdam Study. Hypertension 47: 189–194
Lee JE et al. (2006) Serum uric acid is associated with microalbuminuria in prehypertension. Hypertension 47: 962–967
Diwan SK et al. (2005) Blood pressure response to treadmill testing among medical graduates: the right time to intervene. Indian Heart J 57: 237–240
Fazio S et al. (2005) An exaggerated systolic blood pressure response to exercise is associated with cardiovascular remodeling in subjects with prehypertension. Ital Heart J 6: 886–892
Kokkinos P et al. (2006) Exercise capacity and 24-h blood pressure in prehypertensive men and women. Am J Hypertens 19: 251–258
Barlow CE et al. (2006) Cardiorespiratory fitness is an independent predictor of hypertension incidence among initially normotensive healthy women. Am J Epidemiol 163: 142–150
Vasan RS et al. (2001) Assessment of frequency of progression to hypertension in non-hypertensive participants in the Framingham Heart Study: a cohort study. Lancet 358: 1682–1686
Winegarden CR (2005) From “prehypertension” to hypertension? Additional evidence. Ann Epidemiol 15: 720–725
Zhang H et al. (2006) Progression to hypertension in the non-hypertensive participants in the Flemish Study on Environment, Genes and Health Outcomes. J Hypertens 24: 1719–1727
Qureshi AI et al. (2005) Is prehypertension a risk factor for cardiovascular diseases? Stroke 36: 1859–1863
Chiu YH et al. (2006) Progression of pre-hypertension, stage 1 and 2 hypertension (JNC 7): a population-based study in Keelung, Taiwan (Keelung Community-based Integrated Screening No. 9). J Hypertens 24: 821–828
Washio M et al. (2004) Role of prehypertension in the development of coronary atherosclerosis in Japan. J Epidemiol 14: 57–62
Sipahi I et al. (2006) Effects of normal, pre-hypertensive, and hypertensive blood pressure levels on progression of coronary atherosclerosis. J Am Coll Cardiol 48: 833–838
Vasan RS et al. (2001) Impact of high-normal blood pressure on the risk of cardiovascular disease. N Engl J Med 345: 1291–1297
Baldinger B et al. (2006) Cardiovascular risk factors, BMI and mortality in a cohort of Swiss males (1976-2001) with high-sum-assured life insurance cover. J Insur Med (Seattle) 38: 44–53
Lloyd-Jones DM et al. (2005) Hypertension in adults across the age spectrum: current outcomes and control in the community. JAMA 294: 466–472
Liszka HA et al. (2005) Prehypertension and cardiovascular morbidity. Ann Fam Med 3: 294–299
Mainous AG III et al. (2004) Prehypertension and mortality in a nationally-representative cohort. Am J Cardiol 94: 1496–1500
Greenberg J (2006) Are blood pressure predictors of cardiovascular disease mortality different for prehypertensives than for hypertensives? Am J Hypertens 19: 454–461
Russell LB et al. (2004) Effects of prehypertension on admissions and deaths: a simulation. Arch Intern Med 164: 2119–2124
Kshirsagar AV et al. (2006) Blood pressure usually considered normal is associated with an elevated risk of cardiovascular disease. Am J Med 119: 133–141
Bowman TS et al. (2005) JNC 7 category and risk of cardiovascular death in men: are there differences by age? Am J Geriatr Cardiol 14: 126–131
Hsia J et al. (2007) Prehypertension and cardiovascular disease risk in the Women's Health Initiative. Circulation 115: 855–860
Hansen TW et al. (2007) Cardiovascular outcome in relation to progression to hypertension in the Copenhagen MONICA cohort. Am J Hypertens 20: 483–491
He J et al. (2000) Long-term effects of weight loss and dietary sodium reduction on incidence of hypertension. Hypertension 35: 544–549
Appel LJ et al. (2006) Dietary approaches to prevent and treat hypertension: a scientific statement from the American Heart Association. Hypertension 47: 296–308
Appel LJ et al. (1997) A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med 336: 1117–1124
Sacks FM et al. (2001) Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N Engl J Med 344: 3–9
Whelton SP et al. (2002) Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med 136: 493–503
Xin X et al. (2001) Effects of alcohol reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension 38: 1112–1117
Whelton PK et al. (1998) Sodium reduction and weight loss in the treatment of hypertension in older persons: a randomized controlled trial of nonpharmacologic interventions in the elderly (TONE). TONE Collaborative Research Group. JAMA 279: 839–846
Elmer PJ et al. (2006) Effects of comprehensive lifestyle modification on diet, weight, physical fitness, and blood pressure control: 18-month results of a randomized trial. PREMIER Collaborative Research Group. Ann Intern Med 144: 485–495
Appel LJ et al.; OmniHeart Collaborative Research Group (2005) Effects of protein, monounsaturated fat, and carbohydrate intake on blood pressure and serum lipids: results of the OmniHeart randomized trial. JAMA 294: 2455–2464
He J et al. (2005) Effect of soybean protein on blood pressure: a randomized, controlled trial. Ann Intern Med 143: 1–9
Xu KT and Ragain RM (2005) Effects of weight status on the recommendations of and adherence to lifestyle modifications among hypertensive adults. J Hum Hypertens 19: 365–371
Moore LL et al. (2005) Weight loss in overweight adults and the long-term risk of hypertension: The Framingham Study. Arch Intern Med 165: 1298–1303
Fang J et al. (2005) Exercise and cardiovascular outcomes by hypertensive status: NHANES I epidemiological follow-up study, 1971-1992. Am J Hypertens 18: 751–758
Padilla J et al. (2005) Accumulation of physical activity reduces blood pressure in pre- and hypertension. Med Sci Sports Exercise 37: 1264–1275
The Trials of Hypertension Prevention Collaborative Research Group (1997) Effects of weight loss and sodium reduction intervention on blood pressure and hypertension incidence in overweight people with high-normal blood pressure: The Trials of Hypertension Prevention, Phase II. Arch Intern Med 157: 657–667
Julius S et al. (2006) Feasibility of treating prehypertension with an angiotensin receptor blocker. N Engl J Med 354: 1685–1697
Law MR et al. (2003) Value of low-dose combination treatment with blood pressure-lowering drugs: analysis of 354 randomised clinical trials. BMJ 326: 1427–1431
Vasan RS et al. (2005) Relative importance of borderline and elevated levels of coronary heart disease risk factors. Ann Intern Med 142: 393–402
Prabhakaran D et al. (2005) Cardiovascular risk factor prevalence among men in a large industry of northern India. National Med J India 18: 59–65
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
WJ Elliott has received research grants from Pfizer. He has been on the speakers' bureau or received honoraria from Abbott Laboratories, AstraZeneca, Biovail Pharmaceuticals, Bristol-Myers Squibb, Novartis Pharmaceuticals, Pfizer, Sanofi-Aventis and Sanofi-Synthelabo. He has been a consultant/advisory board member for Biovail Pharmaceuticals, Bristol-Myers Squibb/Sanofi-Aventis and Bristol-Myers Squibb/Sanofi-Synthelabo, Novartis Pharmaceuticals and Pfizer.
HR Black has been on the speakers' bureau or received honoraria from Boehringer Ingelheim, Bristol-Myers Squibb, Daiichi-Sankyo, Forest Laboratories, Novartis Pharmaceuticals, Pfizer, Sanofi-Aventis and Sanofi-Synthelabo. He has been a consultant/advisory board member for Bristol-Myers Squibb/Sanofi-Aventis and Bristol-Myers Squibb/Sanofi-Synthelabo, Daiichi-Sankyo, Forest Laboratories, Gilead, Itercure, Merck, Myogen, Novartis Pharmaceuticals, Pfizer and Sanofi-Aventis.
Rights and permissions
About this article
Cite this article
Elliott, W., Black, H. Prehypertension. Nat Rev Cardiol 4, 538–548 (2007). https://doi.org/10.1038/ncpcardio0989
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1038/ncpcardio0989
This article is cited by
-
‘Inequalities in prevalence of hypertension, prehypertension, anti-hypertensive coverage, awareness, and effective treatment in 429 districts of Iran; a population-based STEPS 2016 small area spatial estimation model’
Journal of Diabetes & Metabolic Disorders (2023)
-
The effect of uric acid and urinary sodium excretion on prehypertension: a nationwide population-based study
BMC Cardiovascular Disorders (2020)
-
Disease trajectory browser for exploring temporal, population-wide disease progression patterns in 7.2 million Danish patients
Nature Communications (2020)
-
The hypertension, diabetes and chronic kidney disease triangle in Arab countries
Journal of Human Hypertension (2017)
-
Effects of heart rate variability biofeedback on cardiovascular responses and autonomic sympathovagal modulation following stressor tasks in prehypertensives
Journal of Human Hypertension (2016)