Abstract
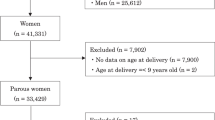
Hypertension in pregnancy is an emerging sex-specific risk factor for cardiovascular disease and may lead to more severe hypertension after pregnancy. The objectives of this study were to investigate the frequency of pregnancy-related hypertension among patients referred to a hypertension clinic and its association with the severity of hypertension and evidence of end-organ damage. In this cross-sectional study, women with hypertension were submitted to a systematic clinical evaluation. The occurrence of pregnancy-related hypertension was investigated by questionnaire. The association between pregnancy-related hypertension and severity of hypertension (stage 2 according to Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC VII)) and end-organ damage was assessed in a logistic regression model. The mean age, systolic and diastolic blood pressure and body mass index (BMI) of the 768 women examined were 51.6±12.7 years, 158.2±26.6 mm Hg, 93.8±14.3 mm Hg and 29.4±5.6 kg/m2, respectively. The proportion of women with pregnancy-related hypertension was 32.9%. It was significantly associated with hypertension at stage 2 (OR: 1.60, 95% CI: 1.14–2.24; P=0.01) after controlling for confounders. The occurrence of a pregnancy-related hypertension was not associated with evidence of optic fundi abnormalities, left ventricular hypertrophy or abnormalities in kidney function. In conclusion, pregnancy-related hypertension is frequent in women referred to a hypertension clinic, and is associated with severe hypertension but not with evidence of end-organ damage.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Bellamy L, Casas JP, Hingorani AD, Williams DJ . Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ 2007; 335: 974.
Sibai B, Dekker G, Kupferminc M . Pre-eclampsia. Lancet 2005; 365: 785–799.
Garovic VD, Hayman SR . Hypertension in pregnancy: an emerging risk factor for cardiovascular disease. Nat Clin Pract Nephrol 2007; 3: 613–622.
Gaio DS, Schmidt MI, Duncan BB, Nucci LB, Matos MC, Branchtein L . Hypertensive disorders in pregnancy: frequency and associated factors in a cohort of Brazilian women. Hypertens Pregnancy 2001; 20: 269–281.
Ray JG, Vermeulen MJ, Schull MJ, Redelmeier DA . Cardiovascular health after maternal placental syndromes (CHAMPS): population-based retrospective cohort study. Lancet 2005; 366: 1797–1803.
Wilson BJ, Watson MS, Pescott GJ, Sunderland S, Campbell DM, Hannaford P, Smith WCS . Hypertensive diseases of pregnancy and risk of hypertension and stroke in later life: results from cohort study. BMJ 2003; 326: 845–849.
Harskamp RE, Zeeman GG . Preeclampsia: at risk for remote cardiovascular disease. Am J Med Sci 2007; 334: 291–295.
Fuchs FD, Wannmacher L, Moraes RS, Moreira LB, Rosito GA, Bercini R et al. A project of an outpatient clinic and follow-up of hypertensive patients: objectives, operating and first results. Rev HCPA 1989; 9: 164–168.
Lubianca JN, Moreira LB, Gus M, Fuchs FD . Stopping oral contraceptives: an effective blood pressure-lowering intervention in women with hypertension. J Hum Hypertens 2005; 19: 451–455.
Fuchs FD, Gus M, Moreira WD, Moreira LB, Moraes RS, Rosito GA et al. Blood pressure effects of antihypertensive drugs and changes in lifestyle in a Brazilian hypertensive cohort. J Hypertens 1997; 15: 783–792.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC VII). JAMA 2003; 289: 2560–2572.
Edhouse J, Thakur RK, Khalil JM . ABC of clinical electrocardiography. Conditions affecting the left side of the heart. BMJ 2002; 324: 1264–1267.
Lubianca JN, Faccin CS, Fuchs FD . Oral contraceptives: a risk factor for uncontrolled blood pressure among hypertensive women. Contraception 2003; 67: 19–24.
Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women's Health Initiative Randomized Controlled Trial. JAMA 2002; 288: 321–333.
Yawn BP, Suman VJ, Jacobsen SJ . Maternal recall of distant pregnancy events. J Clin Epidemiol 1998; 51: 399–405.
Buka SL, Goldstein JM, Spartos E, Tsuang MT . The retrospective measurement of prenatal and perinatal events: accuracy of maternal recall. Schizophr Res 2004; 71: 417–426.
Pouta A, Hartikainen AL, Sovio U, Gissler M, Laitinen J, McCarthy MI et al. Manifestations of metabolic syndrome after hypertensive pregnancy. Hypertension 2004; 43: 825–831.
Fuchs FD, Maestri MK, Bredemeier M, Cardozo SEC, Moreira FC, Wainstein MV et al. Study of the usefulness of optic fundi examination of patients with hypertension in a clinical setting. J Hum Hypertens 1995; 9: 547–551.
Maestri MK, Fuchs SC, Ferlin E, Pakter HM, Nunes G, Moraes RS et al. Detection of arteriolar narrowing in fundoscopic examination: evidence of low performance of direct ophthalmoscopy in comparison with a microdensitometric method. Am J Hypertens 2007; 20: 501–505.
Acknowledgements
This study was partially funded by CNPq and FAPERGS, Brazil.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moreira, L., Gus, M., Nunes, G. et al. Association between pregnancy-related hypertension and severity of hypertension. J Hum Hypertens 23, 415–419 (2009). https://doi.org/10.1038/jhh.2008.140
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhh.2008.140
Keywords
This article is cited by
-
Serotonin risk factors for the development of hypertension in pregnancy
Archives of Gynecology and Obstetrics (2015)
-
Long-Term Effectiveness of Non-Drug Recommendations to Treat Hypertension in a Clinical Setting
American Journal of Hypertension (2012)