Abstract
Background/Objectives:
To examine compensatory changes in sedentary behavior (SB) and light-intensity physical activities (LIPA) in response to a 22-week exercise training program in overweight/obese adults; and to determine if different forms of exercise training and physical activity recommendations interact with these compensatory changes.
Subjects/Methods:
Eighty-nine overweight and obese individuals (body mass index (BMI): 25–34.9 kg/m2, 48% males), aged 18–50 years, were randomized into four intervention groups (strength, endurance, combined strength + endurance and physical activity recommendations) with a 25–30% caloric restriction of total daily energy expenditure for 22 weeks. Energy expenditure was measured by accelerometry before, during and after the program.
Results:
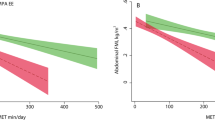
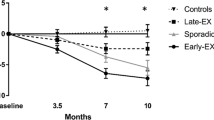
LIPA increased significantly (P<0.001) after three months and at the end of intervention compared to baseline (pre: 281±9 min; 3 months: 303±9 min; post: 312±8 min). SB percentage decreased by 5.3 at the end of the intervention (P=0.002). No interactions were observed between groups or sexes. Significant correlations were found between SB and body weight, fat mass, android fat mass and lean body mass before and after the intervention (P<0.05). LIPA was also significantly correlated with all these body composition variables in the pre-intervention, but only correlated with body weight at the end of intervention.
Conclusions:
There were no compensatory changes after a combined exercise and diet program; where minutes in LIPA increased and %SB decreased after the program, without differences among exercise modes. Greater physical activity levels can contribute to a better percentage and distribution of body tissues.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
The Global BMI Mortality Collaboration. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet 2016; 388: 776–786.
Maher CA, Mire E, Harrington DM, Staiano AE, Katzmarzyk PT . The independent and combined associations of physical activity and sedentary behavior with obesity in adults: NHANES 2003-06. Obesity (Silver Spring) 2013; 21: E730–E737.
Mekary RA, Grontved A, Despres JP, De Moura LP, Asgarzadeh M, Willett WC et al. Weight training, aerobic physical activities, and long-term waist circumference change in men. Obesity (Silver Spring) 2015; 23: 461–467.
Baptista F, Santos DA, Silva AM, Mota J, Santos R, Vale S et al. Prevalence of the Portuguese population attaining sufficient physical activity. Med Sci Sports Exerc 2012; 44: 466–473.
Loprinzi PD, Davis RE . Daily movement patterns and predicted 10-yr risk for a first atherosclerotic cardiovascular disease (ASCVD) event using the pooled cohort risk equations among US adults. Prev Med 2015; 81: 78–81.
Gennuso KP, Gangnon RE, Matthews CE, Thraen-Borowski KM, Colbert LH . Sedentary behavior, physical activity, and markers of health in older adults. Med Sci Sports Exerc 2013; 45: 1493–1500.
Biswas A, Oh PI, Faulkner GE, Bajaj RR, Silver MA, Mitchell MS et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med 2015; 162: 123–132.
Romieu I, Dossus L, Barquera S, Blottiere HM, Franks PW, Gunter M et al. Energy balance and obesity: what are the main drivers? Cancer Causes Control 2017; 28: 247–258.
Chin SH, Kahathuduwa CN, Binks M . Physical activity and obesity: what we know and what we need to know. Obes Rev 2016; 17: 1226–1244.
Thomas DM, Bouchard C, Church T, Slentz C, Kraus WE, Redman LM et al. Why do individuals not lose more weight from an exercise intervention at a defined dose? An energy balance analysis. Obes Rev 2012; 13: 835–847.
King NA, Caudwell P, Hopkins M, Byrne NM, Colley R, Hills AP et al. Metabolic and behavioral compensatory responses to exercise interventions: barriers to weight loss. Obesity (Silver Spring) 2007; 15: 1373–1383.
Smith L, Ekelund U, Hamer M . The potential yield of non-exercise physical activity energy expenditure in public health. Sports Med 2015; 45: 449–452.
Kozey-Keadle S, Staudenmayer J, Libertine A, Mavilia M, Lyden K, Braun B et al. Changes in sedentary time and physical activity in response to an exercise training and/or lifestyle intervention. J Phys Act Health 2014; 11: 1324–1333.
Turner JE, Markovitch D, Betts JA, Thompson D . Nonprescribed physical activity energy expenditure is maintained with structured exercise and implicates a compensatory increase in energy intake. Am J Clin Nutr 2010; 92: 1009–1016.
Willis EA, Herrmann SD, Honas JJ, Lee J, Donnelly JE, Washburn RA . Nonexercise energy expenditure and physical activity in the Midwest Exercise Trial 2. Med Sci Sports Exerc 2014; 46: 2286–2294.
Di Blasio A, Ripari P, Bucci I, Di Donato F, Izzicupo P, D'Angelo E et al. Walking training in postmenopause: effects on both spontaneous physical activity and training-induced body adaptations. Menopause 2012; 19: 23–32.
Melanson EL, Keadle SK, Donnelly JE, Braun B, King NA . Resistance to exercise-induced weight loss: compensatory behavioral adaptations. Med Sci Sports Exerc 2013; 45: 1600–1609.
Washburn RA, Lambourne K, Szabo AN, Herrmann SD, Honas JJ, Donnelly JE . Does increased prescribed exercise alter non-exercise physical activity/energy expenditure in healthy adults? A systematic review. Clin Obes 2014; 4: 1–20.
Melanson EL . The effect of exercise on non-exercise physical activity and sedentary behavior in adults. Obes Rev 2017; 18: 40–49.
Prince SA, Saunders TJ, Gresty K, Reid RD . A comparison of the effectiveness of physical activity and sedentary behaviour interventions in reducing sedentary time in adults: a systematic review and meta-analysis of controlled trials. Obes Rev 2014; 15: 905–919.
American College of Sports Medicine ACSM's Guidelines for Exercise Testing and Prescription. Lippincott Williams & Wilkins: Baltimore, 2006.
Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith BK . American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc 2009; 41: 459–471.
Zapico AG, Benito PJ, Gonzalez-Gross M, Peinado AB, Morencos E, Romero B et al. Nutrition and physical activity programs for obesity treatment (PRONAF study): methodological approach of the project. BMC Public Health 2012; 12: 1100.
Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc 2011; 43: 1334–1359.
Ortega R, Requejo A, Lopez-Sobaler A . Questionniares for dietetic studies and the assessment of nutritional status. In: Requejo A, Ortega R, editor. Nutriguía Manual of Clinical Nutrition in Primary Care. Editoria Complutense: Madrid, 2003.
Johannsen DL, Calabro MA, Stewart J, Franke W, Rood JC, Welk GJ . Accuracy of armband monitors for measuring daily energy expenditure in healthy adults. Med Sci Sports Exerc 2010; 42: 2134–2140.
Camiletti-Moiron D, Segura-Jimenez V, Alvarez-Gallardo IC, Estevez-Lopez F, Aparicio VA, Carbonell-Baeza A et al. Inter-accelerometer comparison to measure physical activity and sedentary time in female fibromyalgia patients: the al-Andalus project. Clin Exp Rheumatol 2015; 33: S46–S52.
Scheers T, Philippaerts R, Lefevre J . Variability in physical activity patterns as measured by the SenseWear Armband: how many days are needed? Eur J Appl Physiol 2012; 112: 1653–1662.
Almeida GJ, Wasko MC, Jeong K, Moore CG, Piva SR . Physical activity measured by the SenseWear Armband in women with rheumatoid arthritis. Phys Ther 2011; 91: 1367–1376.
Wetten AA, Batterham M, Tan SY, Tapsell L . Relative validity of 3 accelerometer models for estimating energy expenditure during light activity. J Phys Act Health 2014; 11: 638–647.
Berntsen S, Hageberg R, Aandstad A, Mowinckel P, Anderssen SA, Carlsen KH et al. Validity of physical activity monitors in adults participating in free-living activities. Br J Sports Med 2010; 44: 657–664.
Feehan LM, Goldsmith CH, Leung AY, Li LC . SenseWearMini and Actigraph GT3X accelerometer classification of observed sedentary and light-intensity physical activities in a laboratory setting. Physiother Can 2016; 68: 116–123.
Calabro MA, Lee JM, Saint-Maurice PF, Yoo H, Welk GJ . Validity of physical activity monitors for assessing lower intensity activity in adults. Int J Behav Nutr Phys Act 2014; 11: 119.
Compagnat M, Daviet JC, Salle JY, Mandigout S, Meurou J, Bordes J . Accelerometers are they accurate for the estimation of total energy expenditure over activities of daily living in stroke survivors? Ann Phys Rehabil Med 2016; 59S: e74.
Almeida GJ, Irrgang JJ, Fitzgerald GK, Jakicic JM, Piva SR . Reliability of physical activity measures during free-living activities in people after total knee arthroplasty. Phys Ther 2016; 96: 898–907.
Huberty J, Ehlers DK, Kurka J, Ainsworth B, Buman M . Feasibility of three wearable sensors for 24 hour monitoring in middle-aged women. BMC Womens Health 2015; 15: 55.
Rosenberger M . Sedentary behavior: target for change, challenge to assess. Int J Obes Suppl 2012; 2: S26–S29.
Sohn MW, Manheim LM, Chang RW, Greenland P, Hochberg MC, Nevitt MC et al. Sedentary behavior and blood pressure control among osteoarthritis initiative participants. Osteoarthritis Cartilage 2014; 22: 1234–1240.
Stamatakis E, Hirani V, Rennie K . Moderate-to-vigorous physical activity and sedentary behaviours in relation to body mass index-defined and waist circumference-defined obesity. Br J Nutr 2009; 101: 765–773.
Hamilton MT, Healy GN, Dunstan DW, Zderic TW, Owen N . Too little exercise and too much sitting: inactivity physiology and the need for new recommendations on sedentary behavior. Curr Cardiovasc Risk Rep 2008; 2: 292–298.
Cleland V, Schmidt M, Salmon J, Dywer T, Venn A . Combined associations of sitting time and physical activity with obesity in young adults. J Phys Act Health 2014; 11: 136–144.
Larsen BA, Allison MA, Kang E, Saad S, Laughlin GA, Araneta MR et al. Associations of physical activity and sedentary behavior with regional fat deposition. Med Sci Sports Exerc 2014; 46: 520–528.
Loprinzi PD . Accelerometer-determined physical activity and mortality in a national prospective cohort study of adults at high risk of a first atherosclerotic cardiovascular disease event. Int J Cardiol 2016; 202: 417–418.
Ryan JM, Crowley VE, Hensey O, Broderick JM, McGahey A, Gormley J . Habitual physical activity and cardiometabolic risk factors in adults with cerebral palsy. Res Dev Disabil 2014; 35: 1995–2002.
Luke A, Bovet P, Plange-Rhule J, Forrester TE, Lambert EV, Schoeller DA et al. A mixed ecologic-cohort comparison of physical activity & weight among young adults from five populations of African origin. BMC Public Health 2014; 14: 397.
McGuire KA, Ross R . Incidental physical activity and sedentary behavior are not associated with abdominal adipose tissue in inactive adults. Obesity (Silver Spring) 2012; 20: 576–582.
Loprinzi PD . Application of the ‘Fat-but-Fit’ paradigm in predicting 10-yr risk for an atherosclerotic cardiovascular disease (ASCVD) event using the pooled cohort risk equations among US adults. Int J Cardiol 2016; 202: 297–299.
O'Donovan G, Kearney E, Sherwood R, Hillsdon M . Fatness, fitness, and cardiometabolic risk factors in middle-aged white men. Metabolism 2012; 61: 213–220.
Cliff DP, Jones RA, Burrows TL, Morgan PJ, Collins CE, Baur LA et al. Volumes and bouts of sedentary behavior and physical activity: associations with cardiometabolic health in obese children. Obesity (Silver Spring) 2014; 22: E112–E118.
Martin A, Fitzsimons C, Jepson R, Saunders DH, van der Ploeg HP, Teixeira PJ et al. Interventions with potential to reduce sedentary time in adults: systematic review and meta-analysis. Br J Sports Med 2015; 49: 1056–1063.
Acknowledgements
The PRONAF Study took place with the financial support of the Ministerio de Ciencia e Innovación, Convocatoria de Ayudas I+D 2008, Proyectos de Investigación Fundamental No Orientada, del VI Plan de Investigación Nacional 2008-2011, (Contrac: DEP2008-06354-C04-01). Special thanks to NKE ‘el niño sarcástico’ for helping and editing our final report. EAC is funded by a pre-doctoral grant of the Coordination for the Improvement of Higher Education Personnel (CAPES). This study is registered at www.clinicaltrials.gov (No. NCT01116856).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Castro, E., Júdice, P., Silva, A. et al. Sedentary behavior and compensatory mechanisms in response to different doses of exercise—a randomized controlled trial in overweight and obese adults. Eur J Clin Nutr 71, 1393–1398 (2017). https://doi.org/10.1038/ejcn.2017.84
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2017.84