Abstract
Liver transplantation is a highly successful treatment, but is severely limited by the shortage in donor organs. However, many potential donor organs cannot be used; this is because sub-optimal livers do not tolerate conventional cold storage and there is no reliable way to assess organ viability preoperatively. Normothermic machine perfusion maintains the liver in a physiological state, avoids cooling and allows recovery and functional testing. Here we show that, in a randomized trial with 220 liver transplantations, compared to conventional static cold storage, normothermic preservation is associated with a 50% lower level of graft injury, measured by hepatocellular enzyme release, despite a 50% lower rate of organ discard and a 54% longer mean preservation time. There was no significant difference in bile duct complications, graft survival or survival of the patient. If translated to clinical practice, these results would have a major impact on liver transplant outcomes and waiting list mortality.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
$199.00 per year
only $3.90 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Change history
23 April 2018
The Source Data files originally published with this article were missing for Extended Data Figures 3 and 4. This has now been corrected.
References
Annual Report on Liver Transplantation 2016/2017 (NHS Blood and Transplant, 2017).
APPHG. Liver disease: today’s complacency, tomorrow’s catastrophe. The All-Party Parliamentary Hepatology Group (APPHG) inquiry into improving outcomes in liver disease. (March, 2014).
Todo, S. et al. Extended preservation of human liver grafts with UW solution. J. Am. Med. Assoc 261, 711–714 (1989).
Clavien, P. A., Harvey, P. R. & Strasberg, S. M. Preservation and reperfusion injuries in liver allografts. An overview and synthesis of current studies. Transplantation 53, 957–978 (1992).
Chouchani, E. T. et al. Ischaemic accumulation of succinate controls reperfusion injury through mitochondrial ROS. Nature 515, 431–435 (2014).
Watson, C. J. et al. Preimplant normothermic liver perfusion of a suboptimal liver donated after circulatory death. Am. J. Transplant. 16, 353–357 (2016).
Mergental, H. et al. Transplantation of declined liver allografts following normothermic ex-situ evaluation. Am. J. Transplant. 16, 3235–3245 (2016).
Perera, T. et al. First human liver transplantation using a marginal allograft resuscitated by normothermic machine perfusion. Liver Transpl. 22, 120–124 (2016).
Ravikumar, R. et al. Liver transplantation after ex vivo normothermic machine preservation: a phase 1 (first-in-man) clinical trial. Am. J. Transplant. 16, 1779–1787 (2016).
Brockmann, J. et al. Normothermic perfusion: a new paradigm for organ preservation. Ann. Surg. 250, 1–6 (2009).
Xu, H. et al. Excorporeal normothermic machine perfusion resuscitates pig DCD livers with extended warm ischemia. J. Surg. Res 173, e83–e88 (2012).
Eisenbach, C. et al. An early increase in gamma glutamyltranspeptidase and low aspartate aminotransferase peak values are associated with superior outcomes after orthotopic liver transplantation. Transplant. Proc 41, 1727–1730 (2009).
Olthoff, K. M. et al. Validation of a current definition of early allograft dysfunction in liver transplant recipients and analysis of risk factors. Liver Transpl 16, 943–949 (2010).
Organ Donation and Transplantation Activity Report 2016/17 (NHS Blood and Transplant, 2017).
Angelico, R. et al. Normothermic machine perfusion of deceased donor liver grafts is associated with improved postreperfusion hemodynamics. Transplant. Direct 2, e97 (2016).
Leithead, J. A. et al. Hepatic ischemia reperfusion injury is associated with acute kidney injury following donation after brain death liver transplantation. Transpl. Int 26, 1116–1125 (2013).
Jay, C. L. et al. Ischemic cholangiopathy after controlled donation after cardiac death liver transplantation: a meta-analysis. Ann. Surg. 253, 259–264 (2011).
Mourad, M. M., Algarni, A., Liossis, C. & Bramhall, S. R. Aetiology and risk factors of ischaemic cholangiopathy after liver transplantation. World J. Gastroenterol. 20, 6159–6169 (2014).
Reddy, S. et al. Non-heart-beating donor porcine livers: the adverse effect of cooling. Liver Transpl. 11, 35–38 (2005).
Abstracts of the 18th Congress of the European Society for Organ Transplantation, 24–27 September 2017, Barcelona, Spain. Transpl. Int. 30 (Suppl 2), 5–576 (2017).
Schulz, K. F., Altman, D. G. & Moher, D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Br. Med. J 340, c332 (2010).
Kootstra, G., Daemen, J. H. & Oomen, A. P. Categories of non-heart-beating donors. Transplant. Proc 27, 2893–2894 (1995).
Makowka, L. et al. Surgical technique of orthotopic liver transplantation. Gastroenterol. Clin. North Am 17, 33–51 (1988).
Glanemann, M. et al. Clinical implications of hepatic preservation injury after adult liver transplantation. Am. J. Transplant 3, 1003–1009 (2003).
Gaffey, M. J. et al. Predictive value of intraoperative biopsies and liver function tests for preservation injury in orthotopic liver transplantation. Hepatology 25, 184–189 (1997).
Karayalçin, K. et al. The role of dynamic and morphological studies in the assessment of potential liver donors. Transplantation 57, 1323–1327 (1994).
Hilmi, I. et al. The impact of postreperfusion syndrome on short-term patient and liver allograft outcome in patients undergoing orthotopic liver transplantation. Liver Transpl 14, 504–508 (2008).
Nasralla, D. et al. A multicentre randomised controlled trial to compare the efficacy of ex-vivo normothermic machine perfusion with static cold storage in human liver transplantation. Protoc. Exch. https://doi.org/10.1038/protex.2018.027 (2018).
Guidelines on Medical Devices. Clinical Investigations: Serious Adverse Event Reporting. Report No. MEDDEV 2.7/3 (European Commission, 2010).
Dindo, D., Demartines, N. & Clavien, P. A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 240, 205–213 (2004).
Acknowledgements
This study was performed by the Consortium for Organ Preservation in Europe (COPE). We thank the European Commission for their support through the Seventh Framework Programme. The following organisations, groups and individuals also made substantial contributions without which this trial could not have been completed successfully: NHS Blood and Transplant; the Surgical Intervention Trials Unit, University of Oxford; the Clinical Trials and Research Governance unit, University of Oxford; Centre for Evidence in Transplantation, Royal College of Surgeons of England; the Liver Transplant Coordinators, anaesthetists and liver unit physicians at the Queen Elizabeth Hospital, Birmingham, Addenbrooke’s Hospital, Cambridge, King’s College Hospital, London, the Royal Free Hospital London, Hospital Clinic, Barcelona, University Hospitals, Leuven, University Hospital, Essen; M. Soo, S. Morrish, C. Morris, L. Randle, R. Macedo Arantes, R. Morovat, A. Elsharkawy, G. Hirschfield, P. Muiesan, J. Isaac, J. Grayer, B. Buchholz, H. Vilca-Melendez, A. Zamalloa, D. Chasiotis, S. Khorsandi, B. Davidson, D. Sharma, A. Esson, D. Monbaliu, S. Mertens, S. Swoboda, J. Neuhaus, T. Benkö, V. Molina, R. Kumar, A. Bradley, M. Laspeyres, B. Patel, A. Mukwamba, S. Banks, the COPE Transplant Technicians, the Specialist Nurses in Organ Donation and, of course, all of the donors and their families. This study was funded by a European Commission Seventh Framework Programme (FP7) Grant (No 305934).
Reviewer information
Nature thanks S. Schneeberger, S. G. Tullius and the other anonymous reviewer(s) for their contribution to the peer review of this work.
Author information
Authors and Affiliations
Consortia
Contributions
D.N., S.R.K., R.J.P., C.C.C. and P.J.F. designed this study with help from other authors. R.J.P is Coordinator of the COPE Consortium. M.Z.A. and R.J.P. oversaw the collection of samples and establishment of the trial biobank. D.N., C.D.L.C., A.W., H.M., M.T.P.R.P., D.M., W.J., N.H., C.I., M.M., R.R., A.J.B., C.J.E.W., I.J., J.P., P.K., A.Pau., M.P. and J.C.G.-V. were responsible for the clinical conduct of the study at the respective trial sites. D.N., S.R.K., V.C. and S.J.D. were responsible for statistical design and analysis. L.R. and C.C.C. provided device support and expertise to all trial sites. D.N., S.U., A.Pal. and J.K. were responsible for MRCP image analysis. P.M., S.R.K. and S.J.D. provided governance oversight to ensure the study adhered to all regulatory and ethical requirements. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
P.J.F. is a co-founder, chief medical officer and consultant to OrganOx Limited and also holds shares in the company. C.C.C. is a co-founder, chief technical officer and consultant to OrganOx Limited and also holds shares in the company. Neither P.J.F. nor C.C.C. were involved in the selection, recruitment or transplantation of patients in this study.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data figures and tables
Extended Data Fig. 1 Forest plot for subgroup analysis of peak AST by donor type.
Geometric mean ratio and 95% confidence interval are reported for each subgroup and overall for all groups. DBD group, n = 87 NMP, n = 80 SCS; DCD group, n = 33 NMP, n = 20 SCS.
Extended Data Fig. 2 Post-reperfusion syndrome.
a, Kaplan–Meier plot for one-year survival of patients with two-sided log-rank test. b, Kaplan–Meier plot for one-year graft survival with two-sided log-rank test.
Extended Data Fig. 3 Machine perfusion parameters during NMP.
a, Hepatic artery flow during NMP. b, Portal vein flow during NMP. c, Perfusate pH during NMP. d, Bile production during NMP. a–d, Data are mean ± s.d. of each time point. Actual values are shown in the table. n = 87.
Extended Data Fig. 4 Perfusate lactate levels during NMP.
Scatter graph with trend line showing perfusate lactate levels at different time points during NMP for all transplanted livers. n = 94.
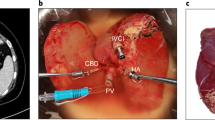
Extended Data Fig. 5 NMP device and circuit.
a, OrganOx metra (generation 1). The NMP device used in the trial. b, OrganOx metra NMP circuit. The liver is perfused via the hepatic artery and portal vein. It drains via the inferior vena cava to a centrifugal pump through which the perfusate passes, via a heat exchanger/oxygenator, to a reservoir or directly into the hepatic artery. The perfusate in the reservoir drains under gravity into the portal vein.
Supplementary information
Supplementary Information
Clinical Trail Protocol. The full trial protocol for a multicentre randomised controlled trial to compare the efficacy of ex-vivo normothermic machine perfusion with static cold storage in human liver transplantation.
Supplementary Information
Statistical Analysis Plan. A comprehensive description of the statistical methodology applied to the trial data.
Supplementary Information
Final Statistical Report. The full report from trial statisticians reporting trial outcomes available at 1 year following completion of recruitment.
Supplementary Information
Primary Non-Function Serious Adverse Event. Clinical trial source document submitted to the trial Data Monitoring Committee providing a narrative description of the events surrounding the transplantation of a normothermic machine perfused liver which resulted in primary non-function of the organ.
Supplementary Information
Device Error Serious Adverse Event. Clinical trial source document submitted to the trial Data Monitoring Committee providing a narrative description of the events surrounding the normothermic machine perfusion of a liver in which a device error led to the organ being discarded.
Rights and permissions
About this article
Cite this article
Nasralla, D., Coussios, C.C., Mergental, H. et al. A randomized trial of normothermic preservation in liver transplantation. Nature 557, 50–56 (2018). https://doi.org/10.1038/s41586-018-0047-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41586-018-0047-9
This article is cited by
-
Comprehensive bile acid pool analysis during ex-vivo liver perfusion in a porcine model of ischemia-reperfusion injury
Scientific Reports (2024)
-
Real-time monitoring of mitochondrial oxygenation during machine perfusion using resonance Raman spectroscopy predicts organ function
Scientific Reports (2024)
-
Comparison of in-gel and in-solution proteolysis in the proteome profiling of organ perfusion solutions
Clinical Proteomics (2023)
-
Vitrification and nanowarming enable long-term organ cryopreservation and life-sustaining kidney transplantation in a rat model
Nature Communications (2023)
-
Normothermic machine perfusion versus static cold storage in donation after circulatory death kidney transplantation: a randomized controlled trial
Nature Medicine (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.