Abstract
Chagas disease, leishmaniasis and sleeping sickness affect 20 million people worldwide and lead to more than 50,000 deaths annually1. The diseases are caused by infection with the kinetoplastid parasites Trypanosoma cruzi, Leishmania spp. and Trypanosoma brucei spp., respectively. These parasites have similar biology and genomic sequence, suggesting that all three diseases could be cured with drugs that modulate the activity of a conserved parasite target2. However, no such molecular targets or broad spectrum drugs have been identified to date. Here we describe a selective inhibitor of the kinetoplastid proteasome (GNF6702) with unprecedented in vivo efficacy, which cleared parasites from mice in all three models of infection. GNF6702 inhibits the kinetoplastid proteasome through a non-competitive mechanism, does not inhibit the mammalian proteasome or growth of mammalian cells, and is well-tolerated in mice. Our data provide genetic and chemical validation of the parasite proteasome as a promising therapeutic target for treatment of kinetoplastid infections, and underscore the possibility of developing a single class of drugs for these neglected diseases.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 51 print issues and online access
$199.00 per year
only $3.90 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Research priorities for Chagas disease, human African trypanosomiasis and leishmaniasis. World Health Organization, WHO Technical Report Series 975, 1–100 (2012)
El-Sayed, N. M. et al. Comparative genomics of trypanosomatid parasitic protozoa. Science 309, 404–409 (2005)
Bilbe, G. Infectious diseases. Overcoming neglect of kinetoplastid diseases. Science 348, 974–976 (2015)
Sundar, S. & Chakravarty, J. An update on pharmacotherapy for leishmaniasis. Expert Opin. Pharmacother. 16, 237–252 (2015)
Nagle, A. S. et al. Recent developments in drug discovery for leishmaniasis and human African trypanosomiasis. Chem. Rev. (2014)
Bern, C. Chagas’ Disease. N. Engl. J. Med. 373, 456–466 (2015)
Chatelain, E. Chagas disease drug discovery: toward a new era. J. Biomol. Screen. 20, 22–35 (2015)
Kennedy, P. G. Clinical features, diagnosis, and treatment of human African trypanosomiasis (sleeping sickness). Lancet Neurol. 12, 186–194 (2013)
Control of the leishmaniases. World Health Organization, WHO Technical Report Series 949, 37–39 (2010)
Yardley, V. & Croft, S. L. A comparison of the activities of three amphotericin B lipid formulations against experimental visceral and cutaneous leishmaniasis. Int. J. Antimicrob. Agents 13, 243–248 (2000)
Dorlo, T. P. et al. Pharmacokinetics of miltefosine in Old World cutaneous leishmaniasis patients. Antimicrob. Agents Chemother. 52, 2855–2860 (2008)
McGwire, B. S. & Satoskar, A. R. Leishmaniasis: clinical syndromes and treatment. QJM 107, 7–14, (2014)
Hotez, P. J. Combating the next lethal epidemic. Science 348, 296–297 (2015)
Sacks, D. & Anderson, C. Re-examination of the immunosuppressive mechanisms mediating non-cure of Leishmania infection in mice. Immunol. Rev. 201, 225–238 (2004)
Nelson, K. G., Bishop, J. V., Ryan, R. O. & Titus, R. Nanodisk-associated amphotericin B clears Leishmania major cutaneous infection in susceptible BALB/c mice. Antimicrob. Agents Chemother. 50, 1238–1244 (2006)
Nunes, M. C. et al. Chagas disease: an overview of clinical and epidemiological aspects. J. Am. Coll. Cardiol. 62, 767–776 (2013)
Coura, J. R. & Borges-Pereira, J. Chagas disease: 100 years after its discovery. A systemic review. Acta Trop. 115, 5–13 (2010)
Bern, C. Antitrypanosomal therapy for chronic Chagas’ disease. N. Engl. J. Med. 364, 2527–2534 (2011)
Viotti, R. et al. Towards a paradigm shift in the treatment of chronic Chagas disease. Antimicrob. Agents Chemother. 58, 635–639 (2014)
Molina, I. et al. Randomized trial of posaconazole and benznidazole for chronic Chagas’ disease. N. Engl. J. Med. 370, 1899–1908 (2014)
Morillo, C. A. et al. Randomized trial of benznidazole for chronic Chagas’ cardiomyopathy. N. Engl. J. Med. 373, 1295–1306 (2015)
Viotti, R. et al. Side effects of benznidazole as treatment in chronic Chagas disease: fears and realities. Expert Rev. Anti Infect. Ther. 7, 157–163 (2009)
Khare, S. et al. Antitrypanosomal treatment with benznidazole is superior to posaconazole regimens in mouse models of Chagas disease. Antimicrob. Agents Chemother. 59, 6385–6394 (2015)
Bustamante, J. M., Bixby, L. M. & Tarleton, R. L. Drug-induced cure drives conversion to a stable and protective CD8+ T central memory response in chronic Chagas disease. Nature Med. 14, 542–550 (2008)
Myburgh, E. et al. In vivo imaging of trypanosome-brain interactions and development of a rapid screening test for drugs against CNS stage trypanosomiasis. PLoS Negl. Trop. Dis. 7, e2384 (2013)
Li, H. et al. Structure- and function-based design of Plasmodium-selective proteasome inhibitors. Nature 530, 233–236 (2016)
Steverding, D. & Wang, X. Trypanocidal activity of the proteasome inhibitor and anti-cancer drug bortezomib. Parasites & Vectors 2, 29 (2009)
Ivens, A. C. et al. The genome of the kinetoplastid parasite, Leishmania major. Science 309, 436–442 (2005)
Li, X. et al. Effect of noncompetitive proteasome inhibition on bortezomib resistance. J. Natl. Cancer Inst. 102, 1069–1082 (2010)
Fernandez, Y. et al. Chemical blockage of the proteasome inhibitory function of bortezomib: impact on tumor cell death. J. Biol. Chem. 281, 1107–1118 (2006)
Zhang, X., Goncalves, R. & Mosser, D. M. The isolation and characterization of murine macrophages. Curr. Protoc. Immunol. Chapter 14, Unit1 4.1 (2008)
Khare, S. et al. Utilizing chemical genomics to identify cytochrome b as a novel drug target for Chagas disease. PLoS Pathog. 11, e1005058 (2015)
Buckner, F. S., Verlinde, C. L., La Flamme, A. C. & Van Voorhis, W. C. Efficient technique for screening drugs for activity against Trypanosoma cruzi using parasites expressing beta-galactosidase. Antimicrob. Agents Chemother. 40, 2592–2597 (1996)
Logan-Klumpler, F. J. et al. GeneDB–an annotation database for pathogens. Nucleic Acids Res. 40, D98–D108 (2012)
Taylor, M. C. & Kelly, J. M. pTcINDEX: a stable tetracycline-regulated expression vector for Trypanosoma cruzi. BMC Biotechnol. 6, 32 (2006)
Hariharan, S., Ajioka, J. & Swindle, J. Stable transformation of Trypanosoma cruzi: inactivation of the PUB12.5 polyubiquitin gene by targeted gene disruption. Mol. Biochem. Parasitol. 57, 15–30 (1993)
Wirtz, E., Leal, S., Ochatt, C. & Cross, G. A. A tightly regulated inducible expression system for conditional gene knock-outs and dominant-negative genetics in Trypanosoma brucei. Mol. Biochem. Parasitol. 99, 89–101 (1999)
Wilk, S. & Chen, W.-E. Purification of the eukaryotic 20S proteasome. Curr. Protoc. Protein Sci. Chapter 21 (2001)
Unno, M. et al. The structure of the mammalian 20S proteasome at 2.75 A resolution. Structure 10, 609–618 (2002)
Melnick, J. S. et al. An efficient rapid system for profiling the cellular activities of molecular libraries. Proc. Natl Acad. Sci. USA 103, 3153–3158 (2006)
Waters, N. J., Jones, R., Williams, G. & Sohal, B. Validation of a rapid equilibrium dialysis approach for the measurement of plasma protein binding. J. Pharm. Sci. 97, 4586–4595 (2008)
Wang, J. & Skolnik, S. Recent advances in physicochemical and ADMET profiling in drug discovery. Chem. Biodivers. 6, 1887–1899 (2009)
Kalvass, J. C., Tess, D. A., Giragossian, C., Linhares, M. C. & Maurer, T. S. Influence of microsomal concentration on apparent intrinsic clearance: implications for scaling in vitro data. Drug Metab. Dispos. 29, 1332–1336 (2001)
Li, C. et al. A modern in vivo pharmacokinetic paradigm: combining snapshot, rapid and full PK approaches to optimize and expedite early drug discovery. Drug Discov. Today 18, 71–78 (2013)
Sacks, D. L. & Melby, P. C. Animal models for the analysis of immune responses to leishmaniasis. Curr. Protoc. Immunol. Chapter 19, Unit 19.12 (2001)
McLatchie, A. P. et al. Highly sensitive in vivo imaging of Trypanosoma brucei expressing “red-shifted” luciferase. PLoS Negl. Trop. Dis. 7, e2571 (2013)
Acknowledgements
This work was supported in part by grants from the Wellcome Trust (091038/Z/09/Z to R.J.G. and F.S., and 104976/Z/14/Z, 104111/15/Z to J.C.M. and E.M.) and NIH (AI106850 to F.S.B.). We thank S. Croft, R. Don, L. Gredsted, A. Hudson and J. Mendlein for discussions, R. Tarleton for T. cruzi CL strain, and G. Cross for T. brucei Lister 427 strain. We thank A. Kreusch for help with proteasome purification, and F. Luna for help with T. cruzi whole-genome sequencing. We acknowledge technical assistance of O. Faghih in generating the plasmids for ectopic expression of PSMB4 in T. cruzi, R. Ritchie for IVIS in vivo imaging, and A. Mak, J. Matzen and P. Anderson for execution of high-throughput screens. We thank J. Isbell and T. Hollenbeck for profiling GNF6702 in ADME assays.
Author information
Authors and Affiliations
Contributions
A.B., F.L., C.J.N.M., P.K.M., A.S.N., J.L.T. and V.Y. designed chemical analogues, and performed chemical synthesis and purification of synthesized analogues. F.S.B., J.B., J.R.G., S.K., H.X.Y.K., Y.H.L., S.P.S.R., F.S. and X.L. conducted and analysed data from in vitro growth-inhibition assays. L.C.D., X.L., J.C.M., E.M., I.C.R., S.P.S.R., M.S., F.S. and B.G.W. conducted and analysed data from in vivo efficacy assays. J.B., M.-Y.G., S.K. and F.S. conducted proteasome purification, proteasome inhibition assays and biochemical data analysis. S.W.B., G.F., S.K., F.S. and J.R.W. designed, conducted and analysed experiments resulting in identification of proteasome resistance mutations. G.S. and B.B. built the homology model of T. cruzi proteasome structure and performed GNF6702 docking. A.B. and J.D.V. analysed T. cruzi proteasome by mass spectrometry. A.N., T.G., M.S., F.S. and T.T. designed, conducted, and analysed PK data. A.N. and V.M. led the chemistry team. F.S. led the biology team. R.J.G. and F.S. supervised and led the overall project, and led the writing of the manuscript. All authors contributed to writing of the manuscript.
Corresponding author
Ethics declarations
Competing interests
Patents related to this work have been filed (WO 2015/095477 A1, WO 2014/151784 A1, WO 2014/151729). Several authors own shares of Novartis.
Additional information
Reviewer Information
Nature thanks M. PhilIips, S. Schreiber and the other anonymous reviewer(s) for their contribution to the peer review of this work.
Extended data figures and tables
Extended Data Figure 1 Pharmacokinetic profile of GNF6702 in mouse.
a, Time profiles of mean free plasma concentration of GNF6702 in mouse model of visceral leishmaniasis; free GNF6702 concentration values were predicted from measured total plasma concentration values collected on day 1 and day 8 of treatment. Dashed blue lines correspond to intra-macrophage L. donovani EC50 of 18 ± 1.8 nM and EC99 of 42 ± 5.6 nM. Circles, means ± s.d.; n = 3 mice for treatment day 1; n = 5 mice for treatment day 8; fraction unbound in mouse plasma = 0.063. For data points lacking error bars, standard deviations are smaller than circles representing means. b, Time course of total GNF6702 concentration in mouse plasma and brain after single oral dose (20 mg kg−1); n = 2 mice per time point; circles, measured values; rectangles, means.
Extended Data Figure 2 GNF6702 clears parasites from mice infected with T. brucei.
a, In vivo quantification of bioluminescent T. brucei in infected mice before and after treatment. i.p., intraperitoneal; day 21, start of treatment; day 28, 24 h after last GNF6702 dose; day 42, evaluation of early parasite recrudescence in mice treated with diminazene aceturate (n = 3); day 42 and 92, absence of parasite recrudescence in mice treated with GNF6702 (n = 6). Images from uninfected mice (3 mice of 4 are shown) aged-matched for day 0 were collected independently using the same acquisition settings. Parasitemia (blue font) and whole mouse total flux (black font) values of each animal are shown above the image; N.D., not detectable. Within each group the mouse numbers in yellow (top left in each image) refer to the same mouse imaged throughout. Complete sets of parasitemia and whole mouse total flux values collected on individual mice throughout the experiment are listed in Supplementary Tables 4 and 5. b, Brains from mice shown in a were soaked in luciferin and imaged for presence of bioluminescent T. brucei at the indicated time points. For three diminazene-treated mice, two images of each brain are shown, one at a lower sensitivity (left) and the other at a high signal intensity scale.
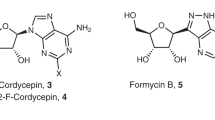
Extended Data Figure 3 Structures and profiles of GNF3943 and GNF8000 used for selection of resistant T. cruzi lines.
Leishmania donovani, amastigotes proliferating within primary mouse macrophages; T. brucei, the bloodstream form trypomastigotes; T. cruzi, amastigotes proliferating in 3T3 fibroblast cells; macrophage, mouse primary peritoneal macrophages; EC50 and CC50, half-maximum growth-inhibition concentration; F, oral bioavailability in mouse after administering single compound dose (20 mg kg−1) as a suspension; CL, plasma clearance in mouse after single i.v. bolus dose (5 mg kg−1); all EC50 and CC50 values correspond to means ± s.e.m. (n = 4 technical replicates).
Extended Data Figure 4 Mutations in proteasome β4 subunit confer resistance to GNF6702 in T. cruzi and T. brucei.
a, Growth curves of wild-type, GNF3943-resistant and GNF8000-resistant T. cruzi epimastigote strains in the presence of increasing concentrations of GNF6702, nifurtimox, bortezomib and MG132; RU (relative units) corresponds to parasite growth relative to the DMSO control (%); for data points lacking error bars, standard errors are smaller than circles representing means; owing to limited aqueous solubility, the highest tested GNF6702 concentration was 10 μM. b, Growth-inhibition EC50 values of GNF6702, bortezomib, MG132 and nifurtimox on indicated T. cruzi strains. c, Growth-inhibition EC50 values of GNF6702 and bortezomib on T. cruzi epimastigotes and T. brucei bloodstream form trypomastigotes overexpressing wild-type PSMB4 or PSMB4F24L. Data shown in panels a, b and c correspond to means ± s.e.m. (n = 3 technical replicates).
Extended Data Figure 5 Correlation between inhibition of parasite proteasome chymotrypsin-like activity and parasite growth inhibition by the GNF6702 compound series.
IC50, half-maximum inhibition of indicated parasite proteasome; T. brucei EC50, half-maximum growth inhibition on T. brucei bloodstream form trypomastigotes; T. cruzi EC50, half-maximum growth inhibition on T. cruzi amastigotes proliferating inside 3T3 cells; data points correspond to means of 2 technical replicates; red circles, IC50 > 20 μM; yellow circles, IC50 > 20 μM and EC50 > 25 μM; data for 317 analogues are shown.
Extended Data Figure 6 Hypothetical model of GNF6702 binding to T. cruzi proteasome β4 subunit.
a, Alignment of amino acid sequences of proteasome β4 subunits (PSMB4) from L. donovani, T. cruzi, T. brucei and Homo sapiens. Green, amino acid residues conserved between human and kinetoplastid PSMB4 proteins; blue, amino acid residues conserved only among kinetoplastid PSMB4 proteins; black, amino acids mutated in T. cruzi mutants resistant to analogues from the GNF6702 series. b, Surface representation of the modelled T. cruzi 20S proteasome structure showing relative positions of the β5 and β4 subunits. β4 amino acid residues F24 and I29 (coloured yellow) are located at the interface of the two β subunits. GNF6702 is depicted in a sphere representation bound into a predicted pocket on the β4 subunit surface with carbon, nitrogen, oxygen and hydrogen atoms coloured magenta, blue, red and grey, respectively. The other T. cruzi 20S proteasome subunits are coloured grey. c, Close-up of the β5 and β4 subunits. The β5 subunit active site (pocket 1, chymotrypsin-like activity) is coloured pale green. The predicted β4 pocket (pocket 2) with bound GNF6702 is coloured blue. The inhibitor is shown in a stick representation with atoms coloured as described in caption for b. β4 residues F24 and I29 are coloured yellow. The proteasome model shown in b and c was produced in the PyMol Molecule Graphics System, Version 1.8, Schrodinger, LLC.
Extended Data Figure 7 Effect of GNF6702 on accumulation of ubiquitylated proteins by T. cruzi epimastigotes and 3T3 cells.
a, Western blot analysis of T. cruzi whole-cell extracts with anti-ubiquitin antibody after treatment with GNF6702 and bortezomib. b, Western blot analysis of 3T3 whole cell extracts with anti-ubiquitin antibody after treatment with GNF6702 and borteomib. c, Concentrations of GNF6702 and bortezomib effecting half-maximum accumulation of ubiquitylated proteins in T. cruzi and 3T3 cells (means ± s.e.m.; n = 3 technical replicates); total ubiquitin signal values in individual blot lanes shown in a and b were quantified and used for calculation of the listed EC50 values. In a and b, numbers above the blot lanes indicate compound concentrations and D indicates control, DMSO-treated cells. For western blot source data, see Supplementary Fig. 1.
Supplementary information
Supplementary Information
Supplementary Information (PDF 399 kb)
Supplementary Tables
This file contains Supplementary Tables 1-11. (XLSX 37 kb)
Rights and permissions
About this article
Cite this article
Khare, S., Nagle, A., Biggart, A. et al. Proteasome inhibition for treatment of leishmaniasis, Chagas disease and sleeping sickness. Nature 537, 229–233 (2016). https://doi.org/10.1038/nature19339
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nature19339
This article is cited by
-
Antimalarial drug discovery: progress and approaches
Nature Reviews Drug Discovery (2023)
-
Quinolone: a versatile therapeutic compound class
Molecular Diversity (2023)
-
A structure-based virtual high-throughput screening, molecular docking, molecular dynamics and MM/PBSA study identified novel putative drug-like dual inhibitors of trypanosomal cruzain and rhodesain cysteine proteases
Molecular Diversity (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.