Abstract
Data sources
Medline/PubMed, Web of Science, Open Grey, Scopus and Cochrane Library databases were searched with no restrictions on dates or language.
Study selection
Randomised controlled clinical trials (RCTs) comparing the effectiveness of HEMA-free and HEMA-containing adhesive systems in NCCL restorations were included.
Data extraction and synthesis
Two reviewers extracted data with risk of bias being assessed using the Cochrane tool. The parameters, retention [RE], marginal adaptation [MA], marginal discoloration [MD], caries [CA], postoperative sensitivity [POS] and overall clinical performance were assessed using a random effects meta-analysis.
Results
Twenty-two studies were included, 13 were at low risk of bias and nine at unclear risk. The number of patients in the studies ranged from 11-124 and study duration ranged from 12 months to 13 years. In all 30 different adhesive systems were tested. For the parameters analysed no significant statistical differences were found between the clinical performances of HEMA-free and HEMA-containing adhesive systems.
Conclusions
HEMA-free and HEMA-containing adhesive systems showed a similar clinical performance in NCCL restorations.
Similar content being viewed by others
Commentary
Since the 1970s, many variants of dental adhesive systems have been developed and produced, with 2-hydroxyethyl methacrylate (HEMA) component playing an important role in many of these adhesive systems. Owing to its high hydrophilicity, HEMA has been introduced to improve the wettability and diffusion into the demineralised collagen fibrils. However, reports of increased water uptake causing hydrolytic degradation of the adhesive interface has driven the manufacturing of HEMA-free adhesives to avoid this negative effect.
The authors of this paper conducted their study to assess the effectiveness of HEMA-free versus HEMA-containing adhesive systems in the restoration of non-carious cervical lesions (NCCLs). NCCLs were selected by the authors as they suggest that they are simple to restore, reducing the effect of operator variability. In addition, they used NCCLs as they are well accepted as an ideal model cavity due to their lack of macromechanical retention and small C-factor.
The paper sets out a clear PICO question as they looked at the clinical performance of composite resin restorations (O) placed in adult patients with NCCLs (P) using HEMA-free adhesive systems (I) versus HEMA-containing adhesive systems (C) to restore these lesions.
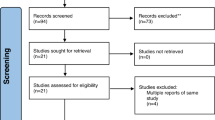
The authors carried out a comprehensive search for relevant randomised controlled clinical trials including the use of Open Grey database for additional unpublished studies. A hand search was also performed and examination of reference lists of included articles was carried out to verify relevant studies were not missed. The search strategy was fully detailed in the report with no restrictions on gender, age, language and publication date. Moreover, data were extracted from the longest follow-up period when reports of the same study with different follow-up periods were found. They also contacted authors of articles with missing or potentially relevant but unreported data weekly via email at least five times. The authors went to considerable efforts to ensure that all relevant papers were identified.
‘Clinical performance of restorations’ was the outcome domain used by the authors to assess treatment effect. This is variously reported in trials as restoration retention, marginal adaptation, marginal discolouration, caries and post-operative sensitivity. This allowed for the inclusion of a larger pool of studies for data extraction with separate meta-analysis being conducted for each sub-outcome. As the authors dichotomised the measurement data for each sub-outcome into ‘acceptable’ or ‘unacceptable’, this means that there is a risk that the review masks degrees of failure which may differ between the two types of bonding agent within the relatively short follow-up periods reported. Follow-up time in the included studies varied from 12 months to 13 years, with 1.5 years to three years being the most common follow-up period. That said, dichotomising their results represents a pragmatic way of combining data when trials use different outcome measurement scales and in many cases is the only way in which data from such RCTs can be combined in meta-analysis.
It is worthy to note that there were no systematic reviews prior to this one which evaluated the influence of a specific component within dental adhesive systems. However, the authors acknowledge that there may be other differences between the bonding agents that were used which is not accounted for in the analysis. It is assumed that any difference detected would be due to the presence or absence of HEMA alone. That said, the authors also highlighted that only patients with no parafunctional habits, normal dietary habits, good periodontal health and with opposing natural dentition were included. This approach controls for these possible confounding factors and allows for comparison of the relative effect of each type of bond. However, as such favourable characteristics are not always present during routine dental care, it could result in an overestimation of absolute benefit for both types of bond when compared with a ‘real world’ setting.
Accepting the limitations of primary studies, the meta-analysis carried out in this review allows the authors to conclude that HEMA-free adhesive systems do not appear to have better clinical performance of NCCL restorations than HEMA-containing systems when used to restore NCCLs in adults. However, some would argue that these lesions need not be restored at all, but monitored instead. In some ways, that is not the question being addressed here as the NCCLs are being used as a model cavity. To what extent the results of this review can be applied to other applications of these bonding agents is unclear.
Author information
Authors and Affiliations
Additional information
Address for correspondence: TaiÏse Sousa Pamplona da Silva, Departamento de DentiÏstica, Faculdade de Odontologia, Universidade Federal do ParaÏ, Rua Augusto Corrêa, 1, GuamaÏ, CEP 66075-110, BeleÏm, PA, Brazil. E-mail: taisepam@yahoo.com.br (T.S.P. da Silva)
da Silva TSP, de Castro RF, Magno MB, Maia LC, Silva E Souza MHD Júnior. Do HEMA-free adhesive systems have better clinical performance than HEMA-containing systems in noncarious cervical lesions? A systematic review and meta-analysis. J Dent 2018 Jul; 74: 1-14. doi:10.1016/j.jdent.2018.04.005. Epub 2018 Apr 9.Review. PubMed PMID: 29649505.
Rights and permissions
About this article
Cite this article
Sia, C., Levey, C. HEMA-free or HEMA-containing adhesive systems for non-carious cervical lesions. Evid Based Dent 19, 114–115 (2018). https://doi.org/10.1038/sj.ebd.6401345
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ebd.6401345