Summary:
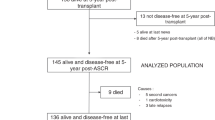
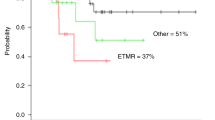
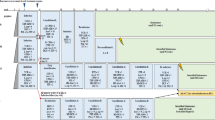
Primary brain tumours, a heterogeneous group of cancer that constitute the second most common cancer in childhood, were historically treated with neurosurgical resection and radiation therapy. Chemotherapy has proven to be beneficial for some histological types, which has since led to exploration of the role of high-dose chemotherapy and haematopoietic stem cell rescue. Patients with high-grade glial tumours, primitive neuroectodermal tumours and high-risk medulloblastoma usually fare poorly. The indicators of bad prognosis are metastatic status, extent of resection and age. Children <3 years at diagnosis carry worse prognosis. Rare cancers such as ependymoblastoma, atypical teratoid rhabdoid tumour and choroid plexus carcinoma have a dismal prognosis regardless of the above-mentioned indicators. The use of myeloablative therapy (MAT) has been investigated to improve the rate of long-term DFS, as well as to reduce and delay in the youngest children the use of the craniospinal irradiation associated with unacceptable late effects. We will overview the literature regarding patients with ‘good and uncertain indications’ to MAT. Ependymoma and brain stem tumours, for which the available data discourage the use of MAT, are excluded. Finally, we will summarize a single Institution experience (Giannina Gaslini Children's Hospital, Genoa) with MAT in the period 1997–2003.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Dunkel IJ, Finlay JL . High-dose chemotherapy with autologous stem cell rescue for brain tumours. Crit Rev Oncol/Hematol 2002; 41: 197–204.
Gardner SL . Application of stem cell transplant for brain tumours. Pediatr Transplant 2004; 8 (Suppl 5): 28–32.
Heideman RL, Douglass EC, Krance RA et al. High-dose chemotherapy and autologous bone marrow rescue followed by interstitial and external-beam radiotherapy in newly diagnosed pediatric malignant gliomas. J Clin Oncol 1993; 11: 1458–1465.
Mason WP, Grovas A, Halpern S et al. Intensive chemotherapy and bone marrow rescue for young children with newly diagnosed malignant brain tumors. J Clin Oncol 1998; 16: 210–221.
Strother D, Ashley D, Kellie SJ et al. Feasibility of four consecutive high-dose chemotherapy cycles with stem-cell rescue for patients with newly diagnosed medulloblastoma or supratentorial primitive neuroectodermal tumor after craniospinal radiotherapy: results of a collaborative study. J Clin Oncol 2001; 19: 2696–2704.
Garrè ML, Massimino M, Cefalo G et al. High risk malignant CNS tumours in infants: standard vs myeloablative chemotherapy. The experience of the Italian co-operative study for children <3 years of age. Oral Presentation at 10th International Symposium on Paediatric Neuro-Oncology, London, 9–12 June 2002.
Garrè ML, Dallorso S, Milanaccio C et al. Myeloablative chemotherapy with peripheral blood stem cells rescue before craniospinal radiotherapy, in patients with medulloblastoma with post-operative residual or metastatic disease. Results of a mono-institutional study in Italy. Oral Presentation at 11th International Symposium on Paediatric Neuro-Oncology, Boston, 13–16 June 2004.
Evans AE, Jenkin RD, Sposto R et al. The treatment of medulloblastoma. Results of a prospective randomized trial of radiation therapy with and without CCNU, vincristine, and prednisone. J Neurosurg 1990; 72: 572–582.
Bailey CC, Gnekow A, Wellek S et al. Prospective randomised trial of chemotherapy given before radiotherapy in childhood medulloblastoma. International Society of Paediatric Oncology (SIOP) and the German Society of Paediatric Oncology (GPO): SIOP II. Med Pediatr Oncol 1995; 25: 166–178.
Belza MG, Donaldson SS, Steinberg GK et al. Medulloblastoma: freedom from relapse longer than 8 years – a therapeutic cure? J Neurosurg 1991; 75: 575–582.
Torres CF, Rebsamen S, Silber JH et al. Surveillance scanning of children with medulloblastoma. N Engl J Med 1994; 330: 892–895.
Dupuis-Girod S, Hartmann O, Benhamou E et al. Will high dose chemotherapy followed by autologous bone marrow transplantation supplant cranio-spinal irradiation in young children treated for medulloblastoma? J Neurooncol 1996; 27: 87–98.
Dunkel IJ, Boyett JM, Yates A et al. High-dose carboplatin, thiotepa, and etoposide with autologous stem-cell rescue for patients with recurrent medulloblastoma. J Clin Oncol 1998; 16: 222–228.
Pérez-Martinez A, Quinterno V, Gonzalez Vicent M et al. High-dose chemotherapy with autologous stem cell rescue as first line treatment in young children with medulloblastoma and supratentorial primitive neuroectodermal tumors. J Neuro-Oncol 2004; 67: 101–106.
Broniscer A, Nicolaides TP, Dunkel IJ et al. High-dose chemotherapy with autologous stem-cell rescue in the treatment of patients with recurrent non-cerebellar primitive neuroectodermal tumors. Pediatr Blood Cancer 2004; 42: 261–267.
Gururangan S, McLaughlin C, Quinn J et al. High-dose chemotherapy with autologous stem-cell rescue in children and adults with newly diagnosed pinealoblastomas. J Clin Oncol 2003; 21: 2187–2191.
Biron P, Vial C, Chauvin F et al. Strategy including surgery, high dose BCNU followed by ABMT and radiotherapy in supratentorial high grade astrocytomas: a report of 98 patients. In: Dicke KA, Armitage JO, Dicke-Evinger MJ (eds.). Autologous Bone Marrow Transplantation: Proceedings of the Fifth International Symposium. University of Nebraska Medical Center: Omaha, 1991, pp 637–645.
Durando X, Lemaire JJ, Tortochaux J et al. High-dose BCNU followed by autologous hematopoietic stem cell transplantation in supratentorial high-grade malignant gliomas: a retrospective analysis of 114 patients. Bone Marrow Transplant 2003; 31: 559–564.
Bouffet E, Mottolese C, Jouvet A et al. Etoposide and thiotepa followed by ABMT (autologous bone marrow transplantation) in children and young adults with high-grade gliomas. Eur J Cancer 1997; 33: 91–95.
Finlay JL, Goldman S, Wang MC et al. Pilot study of high-dose thiotepa and etoposide with autologous bone marrow rescue in children and young adults with recurrent CNS tumors. J Clin Oncol 1996; 14: 2495–2503.
Grovas AC, Boyett JM, Lindsley K et al. Regimen-related toxicity of myeloablative chemotherapy with BCNU, thiotepa, and etoposide followed by autologous stem cell rescue for children with newly diagnosed glioblastoma multiforme: report from the Children's Cancer Group. Med Pediatr Oncol 1999; 33: 83–87.
Rorke LB, Packer RJ, Biegel JA . Central nervous system atypical teratoid/rhabdoid tumors of infancy and childhood: definition of an entity. J Neurosurg 1996; 85: 56–65.
Garrè ML, Abate ME, Giangaspero F et al. Clinical features and treatment (TX) of CNS atypical theratoid/rhabdoid tumour (AT/RT). Invited Lecture at XXXIV SIOP Meeting, Porto 18–21 September 2002. Med Pediatr Oncol 2002; 39: 275.
Dallorso S, Rivabella L, Cefalo G et al. Technical aspects and feasibility of peripheral blood progenitor cell (PBPC) collection in 20 cases of infants with Central Nervous System (CNS) tumours treated with myeloablative therapy. Oral Presentation at 10th International Symposium on Paediatric Neuro-Oncology, London, 9–12 June 2002.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Dallorso, S., Dini, G., Ladenstein, R. et al. Evolving role of myeloablative chemotherapy in the treatment of childhood brain tumours. Bone Marrow Transplant 35 (Suppl 1), S31–S34 (2005). https://doi.org/10.1038/sj.bmt.1704841
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1704841