Computer illustration of B cells producing monoclonal antibodies. The anti-cancer drugs panitumumab and bevacizumab are monoclonal antibodies that target different molecular pathways.© Nanoclustering/Science Photo Library/Getty
A long-standing debate over the most effective treatment for prevalent forms of colorectal cancer — the world’s third most diagnosed cancer — was finally settled in June 2022. The much-anticipated results of a trial of more than 800 participants in Japan revealed that, when coupled with standard chemotherapy, the drug panitumumab lowered the risk of death by 18% compared to bevacizumab, another drug commonly paired with chemotherapy for certain patients. Takayuki Yoshino of the National Cancer Center Hospital East (NCCHE) in Kashiwa, Japan, reported the results at the plenary session of the 2022 Annual Meeting of the American Society of Clinical Oncology (ASCO) in Chicago, one of the most prominent conferences in the field1,2.
“Colorectal-cancer researchers have waited nearly a decade to obtain definitive evidence on the effectiveness of panitumumab versus bevacizumab,” says Yoshino. “The results have led to a change in treatment guidelines issued by both ASCO and the National Comprehensive Cancer Network, affecting the course of treatment for as many as 200,000 patients around the world.”
New findings
Surgical removal of tumours is the gold standard for the first treatment in colorectal cancer, but more than a third of patients have inoperable tumours when diagnosed. For about half of these patients, namely those who have a non-mutated version of the RAS gene, panitumumab or bevacizumab combined with chemotherapy are treatment options. Pairing either panitumumab or bevacizumab with chemotherapy prolongs overall survival by up to 30 months.
Panitumumab and bevacizumab are antibodies that target different molecular pathways: panitumumab inhibits the epidermal growth factor receptor, whereas bevacizumab inhibits the vascular endothelial growth factor. But there had been mixed evidence over which of the two was the most effective treatment.
“The two drugs had been compared directly once in the US and once in Europe. However, these trials had been conducted when we knew less about the RAS family of genes. Back then, we only knew that mutations in KRAS exon 2 were relevant,” explains Yoshino. “Retrospective analyses of these trials showed conflicting results. The European study suggested that panitumumab was superior. On the other hand, analyses of the US one yielded insignificant results. Therefore, panitumumab was more widely used in Europe, whereas bevacizumab was mostly used in the US.”
Yoshino, along with Takeda Pharmaceutical, launched the current study, known as PARADIGM (Panitumumab and RAS, Diagnostically useful Gene Mutation for mCRC) trial, to compare panitumumab and bevacizumab directly in patients with non-mutated versions of RAS genes. “It also became clear from basic research that panitumumab worked better for tumours originating on the left side of the colon; our trial protocol was able to account for these new findings,” says Yoshino. “Now, with strong evidence in favour of panitumumab, we anticipate treatments for left-sided colorectal cancers to be standardized worldwide.”
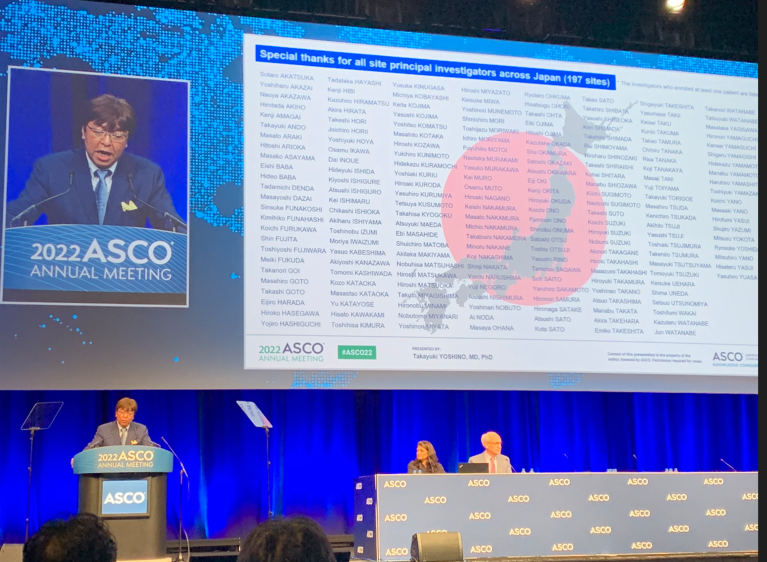
Takayuki Yoshino reporting the findings of a major Japanese study into the effectivenesses of panitumumab and bevacizumab for treating colorectal cancer at the 2022 Meeting of the American Society of Clinical Oncology.© Takeda Pharmaceutical Company Limited
Bigger questions
The PARADIGM trial was one of the largest studies of its kind to have been conducted in Asia. “We worked with nearly 200 hospitals across Japan. With their generous support, we gathered as many as 800 participants in two years and a month — a record-breaking feat,” says Junpei Soeda, head of Medical Affairs at Takeda Pharmaceutical’s Japan Oncology Business Unit, which distributes panitumumab in Japan.
The impact of the PARADIGM trial reaches far beyond establishing evidence for the panitumumab’s superiority. The dataset from the PARADIGM trial will be integrated into a database managed under the ARCAD-Asia project. Launched in 2021, the project facilitates the sharing of clinical trial data on colorectal cancer across Asia.
ARCAD-Asia works in conjunction with the ARCAD Advanced Colorectal Cancer Project, established in 2009 jointly by the French ARCAD Foundation and the US Mayo Clinic to facilitate international data sharing. Collectively, the databases developed by ARCAD and ARCAD-Asia store information collected from nearly 43,000 patients, and includes anything from industry-sponsored trials conducted to obtain drug approval, to academia-led clinical trials aimed at optimizing therapy.
Scanning electron micrograph of a cancer cell in the colon.© Micro Discovery/ Corbis Documentary/Getty
“There are clinical research questions that we cannot answer with a sample of 800 patients, but can with 43,000,” explains Soeda. “Most notably, analyses of progression-free survival — the time that elapses without the cancer worsening — that utilized this massive dataset have led to new drug approvals in some countries.
The ARCAD-Asia project will make data collected in Asia more available globally. “The launch of ARCAD-Asia was a significant milestone as it made Asian clinical trial data available for the world to use,” says Yoshino. “However, Asian clinical trials constitute less than a tenth of the available data in the ARCAD partnership. Studies like PARADIGM help enrich the database with high-quality information.”
In addition, Takeda has funded another study in parallel to PARADIGM trial to investigate medical signs and molecular indicators related to colorectal cancer. “We’ve been collecting cell-free DNA and circulating tumour DNA in blood plasma, as well as tumour tissue samples from patients involved in PARADIGM before and after treatment,” explains Soeda, “This is to run large-scale analyses of indicators are predictive of colorectal cancer or resistance to treatment.”
Yoshino has high hopes for Takeda’s research to uncover valuable new insights. “Takeda has collected plasma and tissue from more than 90% of patients after treatment — collecting 50% is already an achievement in global clinical trials,” he says. “There’s so much we can expect from the comprehensive analyses that they have planned.”
Working together
“Takeda has been committed to several types of cancer related industry–academia collaboration projects and will further enhance collaboration which can embody Takeda Japan Oncology Business Unit Policy such as utilization of data and digital for accelerating patients access to medicine and promoting personalized genomic medicine,” explains Yukiko Sakakibara, head of Strategic Portfolio Planning in Takeda’s Japan Oncology Business Unit.
One of the examples between industry and academia also create foundations for high-impact oncology research in Japan, says Yoshino. “SCRUM-Japan MONSTAR-SCREEN, a cancer-genome-screening project led by NCCHE, has been incredibly successful — more than 200 medical institutions and nearly 20 industry partners are contributing as collaborators,” he explains.
Patients enrolled in the project have free access to genetic screening, while the analysis results and data on treatment are shared with participating institutions. So far, the project has more than 30,000 patients enrolled, and it has resulted in the approval of eleven new drugs and seven diagnostics.
“Collaborations between industry and academia in Japan are making real-world impacts on an international scale,” notes Yoshino. “And this is only the beginning.”



 Nature Index Japan 2023
Nature Index Japan 2023